What is endometrial stroma? It’s a vital component of the uterus, often overlooked but playing a critical role in the complex dance of the menstrual cycle. This intricate tissue, nestled within the uterine lining, is a dynamic powerhouse responsible for supporting the growth of the endometrium, providing a welcoming environment for a fertilized egg, and responding to the delicate symphony of hormones that govern a woman’s reproductive health.
Endometrial stroma is a complex network of cells and extracellular matrix, a hidden world within the uterus that is constantly adapting and changing. It is the foundation upon which the endometrial lining builds and rebuilds each month, a testament to the remarkable resilience of the female reproductive system.
Endometrial Stroma in Health and Disease
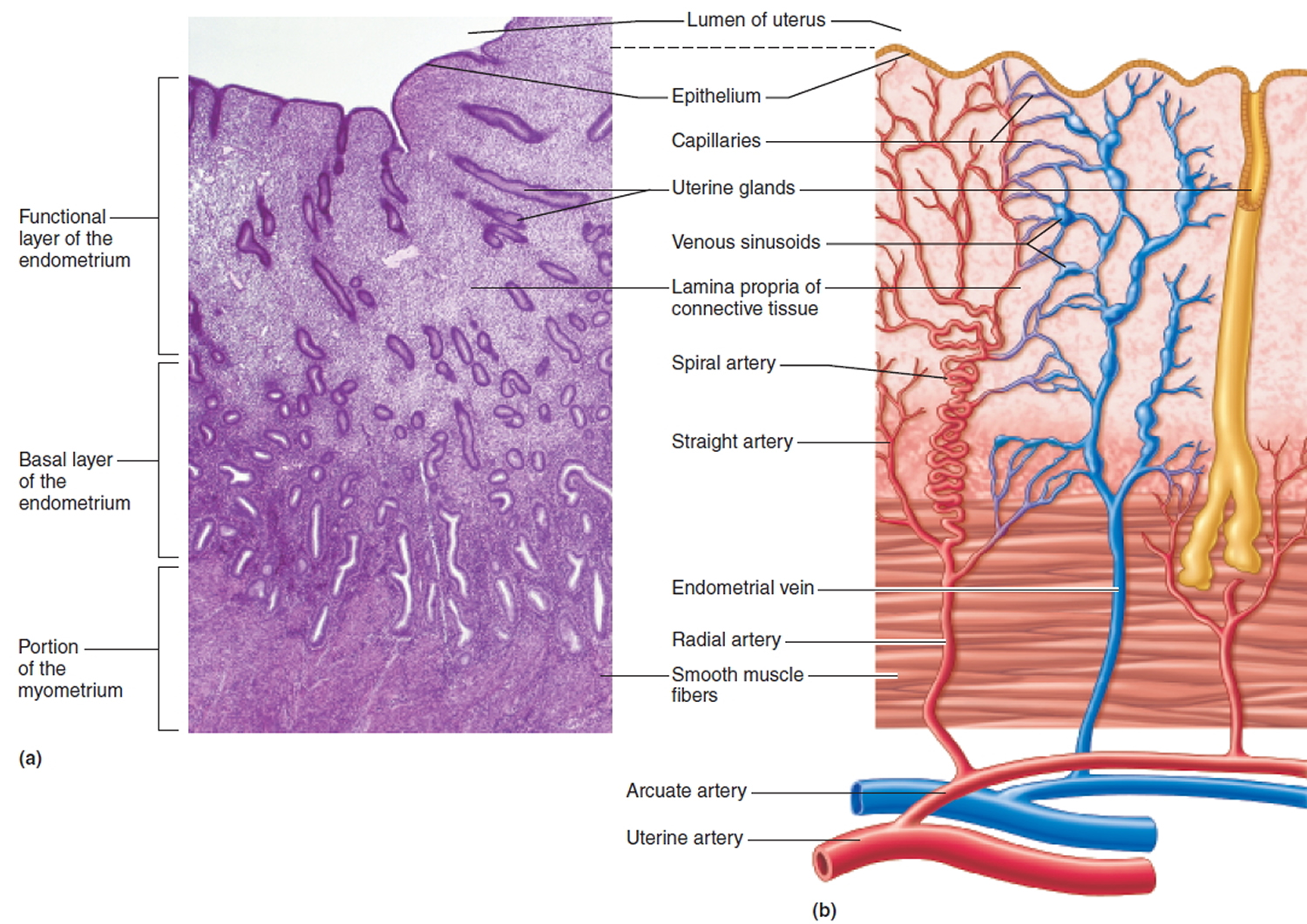
The endometrial stroma, the connective tissue component of the endometrium, plays a crucial role in supporting and regulating the functional layer of the endometrium, which undergoes cyclical changes during the menstrual cycle. Understanding the structural and functional differences in the endometrial stroma between a healthy uterus and in disease states like endometriosis and uterine fibroids is vital for comprehending the pathogenesis of these conditions.
Endometrial Stroma in Health and Disease, What is endometrial stroma
The endometrial stroma in a healthy uterus exhibits a well-organized structure, consisting of fibroblasts, smooth muscle cells, blood vessels, and extracellular matrix components. It is responsible for providing structural support to the endometrial epithelium, facilitating nutrient and oxygen exchange, and participating in the cyclical changes of the endometrium during the menstrual cycle. In endometriosis, endometrial-like tissue grows outside the uterus, often in the pelvic cavity.
The endometrial stroma in endometriosis is characterized by several notable changes:
- Increased Cellular Density: The endometrial stroma in endometriosis exhibits a higher density of cells, particularly fibroblasts, compared to the normal endometrium.
- Abnormal Cell Morphology: Endometrial stromal cells in endometriosis often display atypical morphology, including increased nuclear size and altered chromatin patterns.
- Increased Vascularity: The endometrial stroma in endometriosis is typically hypervascular, with an increased number of blood vessels.
- Elevated Inflammatory Markers: The stromal cells in endometriosis often express elevated levels of inflammatory mediators, contributing to the chronic inflammatory environment associated with this condition.
The altered structure and function of the endometrial stroma in endometriosis contribute to the characteristic symptoms of the disease, including pain, infertility, and adhesions. The exact mechanisms underlying these changes are not fully understood, but hormonal imbalances, immune dysregulation, and genetic factors are thought to play a role.
Endometrial Stroma and Uterine Fibroids
Uterine fibroids, benign tumors of the uterine muscle, are often associated with changes in the endometrial stroma. While the exact role of the endometrial stroma in fibroid development is still being investigated, several studies suggest a potential link:
- Stromal Cell Proliferation: Some studies suggest that stromal cells in the vicinity of fibroids may exhibit increased proliferation rates, contributing to the growth of the fibroid.
- Cytokine Production: Stromal cells in fibroids may produce elevated levels of cytokines, which can promote angiogenesis (new blood vessel formation) and contribute to fibroid growth.
- Extracellular Matrix Remodeling: The endometrial stroma in fibroids may undergo changes in the composition and organization of the extracellular matrix, which can influence fibroid growth and development.
Further research is needed to elucidate the precise mechanisms by which the endometrial stroma contributes to the development and progression of uterine fibroids. However, understanding the role of the endometrial stroma in these conditions could lead to the development of novel therapeutic strategies.
Hormonal Imbalances and Endometrial Stroma
The endometrial stroma is highly responsive to hormonal fluctuations, particularly estrogen and progesterone. Hormonal imbalances can significantly impact the structure and function of the endometrial stroma, contributing to various gynecological conditions.
- Estrogen Dominance: Excess estrogen levels can lead to increased endometrial stromal cell proliferation and vascularity, which can contribute to conditions like endometriosis and uterine fibroids.
- Progesterone Deficiency: Insufficient progesterone levels can disrupt the normal cyclical changes of the endometrial stroma, leading to irregular bleeding, infertility, and an increased risk of endometrial hyperplasia (overgrowth of the endometrial lining).
- Polycystic Ovary Syndrome (PCOS): PCOS, a hormonal disorder characterized by androgen excess and insulin resistance, can also affect the endometrial stroma, leading to irregular menstrual cycles, endometrial thickening, and an increased risk of endometrial cancer.
Managing hormonal imbalances through lifestyle modifications, medication, or hormone therapy can help regulate the structure and function of the endometrial stroma and mitigate the associated health risks.
Research and Future Directions

The endometrial stroma plays a crucial role in female reproductive health, and ongoing research continues to unravel its complex functions and potential therapeutic applications. Understanding the intricate interplay between the stroma and other endometrial components, including the epithelium and immune cells, is essential for developing innovative approaches to address reproductive challenges.
Potential Applications in Fertility Treatments
The intricate interplay between the endometrial stroma and other endometrial components, such as the epithelium and immune cells, makes it a promising target for fertility treatments. Research is exploring various strategies to manipulate the endometrial stroma to enhance implantation and improve pregnancy outcomes.
- Stromal Cell Transplantation: Stromal cells, derived from the endometrium, are being investigated for their potential to improve endometrial receptivity and support embryo implantation. Studies have shown that transplantation of stromal cells can enhance the thickness and vascularization of the endometrium, creating a more favorable environment for implantation. This approach is particularly promising for women with thin endometrium or other endometrial abnormalities.
- Stromal Cell-Based Therapies: Stromal cells possess regenerative properties and can secrete factors that promote endometrial growth and angiogenesis. Researchers are exploring the use of stromal cells to develop novel therapies for conditions like endometriosis, where abnormal endometrial tissue growth occurs outside the uterus. These therapies could potentially reduce pain and improve fertility in women with endometriosis.
- Targeted Drug Delivery: The endometrial stroma is a potential target for targeted drug delivery systems aimed at improving endometrial receptivity. Researchers are developing nanocarriers and other delivery systems that can specifically target stromal cells, delivering drugs or growth factors that enhance endometrial function. This approach could potentially improve implantation rates and reduce the need for invasive procedures.
Emerging Technologies and Techniques
Advances in technology and research techniques are revolutionizing our understanding of the endometrial stroma and its role in reproductive health. These innovations are paving the way for more precise and personalized approaches to diagnosis and treatment.
- Single-Cell RNA Sequencing: This technique allows researchers to analyze gene expression at the level of individual cells within the endometrial stroma. By studying the transcriptome of individual stromal cells, researchers can gain insights into the heterogeneity of the stroma and identify specific cell populations involved in endometrial function. This information can be used to develop targeted therapies for specific endometrial disorders.
- Organoid Culture: Organoids are three-dimensional cell cultures that mimic the structure and function of tissues and organs. Endometrial organoids provide a powerful tool for studying stromal-epithelial interactions and the effects of various stimuli on endometrial function. These organoids can be used to screen potential drug candidates and investigate the mechanisms underlying endometrial diseases.
- Biomarkers: Researchers are identifying specific biomarkers within the endometrial stroma that can be used to predict endometrial receptivity and diagnose endometrial disorders. These biomarkers can be measured in blood or endometrial biopsies, providing valuable information about the health and function of the endometrium.
The intricate world of endometrial stroma is a captivating journey through the heart of the uterus. From its cellular composition and dynamic extracellular matrix to its crucial role in supporting the endometrial lining and responding to hormonal cues, endometrial stroma is a testament to the remarkable complexity and delicate balance of the female reproductive system. Understanding this hidden hero offers valuable insights into reproductive health and sheds light on the intricate processes that govern a woman’s life.
Query Resolution: What Is Endometrial Stroma
What are the potential implications of endometrial stroma abnormalities?
Abnormalities in endometrial stroma can contribute to conditions like endometriosis, uterine fibroids, and infertility. Research is ongoing to understand these connections and develop targeted treatments.
How does endometrial stroma change during pregnancy?
During pregnancy, endometrial stroma undergoes significant changes, becoming more vascular and supporting the growth of the placenta. These changes are crucial for nourishing the developing fetus.
Is there a specific diet that can benefit endometrial health?
While no specific diet can directly impact endometrial health, maintaining a balanced diet rich in fruits, vegetables, and whole grains is essential for overall health and may indirectly support reproductive function.
Can endometrial stroma be affected by stress?
Chronic stress can disrupt hormonal balance, potentially impacting endometrial function. Managing stress through healthy coping mechanisms is crucial for overall well-being and reproductive health.






