What is central echogenic stroma? This term, often encountered in ultrasound reports, refers to a bright, reflective area within the uterus that can be visualized during a prenatal scan. While it might sound alarming, central echogenic stroma is frequently a normal finding, particularly during the early stages of pregnancy. However, it can also be associated with certain conditions, making it essential to understand its significance and potential implications.
Central echogenic stroma appears as a bright, white spot on the ultrasound image, often located within the uterine cavity. It’s composed of dense connective tissue and blood vessels, which contribute to its echogenic (reflective) nature. This structure plays a crucial role in supporting the developing embryo and placenta, but its presence can sometimes raise concerns about potential complications.
Definition of Central Echogenic Stroma
Imagine your uterus as a complex and intricate organ, constantly evolving throughout your life. Inside this organ, there are many different structures, each with its own unique purpose. One of these structures is the central echogenic stroma, which plays a crucial role in the development of your baby during pregnancy.Central echogenic stroma is a small, bright spot that appears on an ultrasound image of the uterus.
It’s like a tiny beacon, signaling the presence of a specific area within the uterus. This bright spot represents a dense collection of cells that are responsible for providing nutrients and support to the developing embryo.
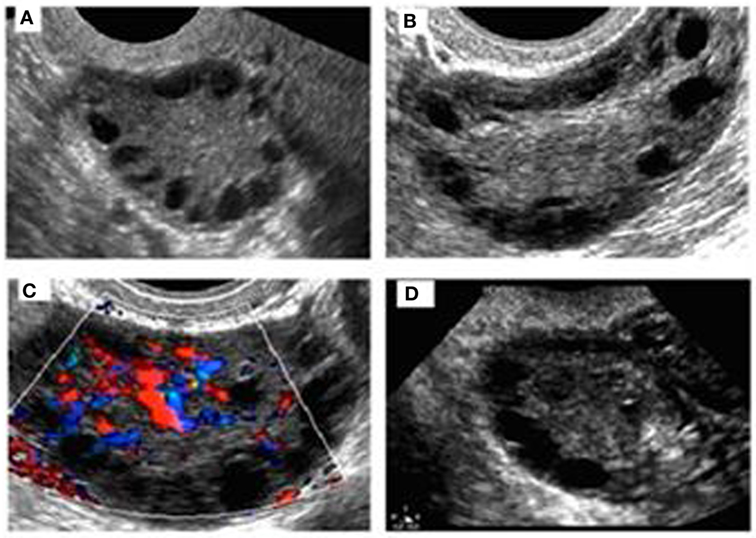
Appearance of Central Echogenic Stroma on Ultrasound
Central echogenic stroma is characterized by its bright, white appearance on an ultrasound image. This brightness is due to the dense nature of the cells within this structure. It typically appears as a small, round or oval-shaped structure located in the center of the uterus.
Comparison of Central Echogenic Stroma with Other Echogenic Structures
While central echogenic stroma is a common finding on ultrasound images, it’s important to differentiate it from other echogenic structures that might be present in the uterus. Here’s a comparison of central echogenic stroma with other echogenic structures:
| Structure | Appearance on Ultrasound | Location ||—|—|—|| Central echogenic stroma | Small, bright, round or oval-shaped | Center of the uterus || Fibroids | Large, irregular, often multiple | Can be located anywhere in the uterus || Polyps | Small, smooth, often attached to the uterine wall | Can be located anywhere in the uterus || Endometrial thickening | Thickening of the uterine lining | Throughout the uterine cavity |
The appearance of central echogenic stroma on ultrasound is distinct from other echogenic structures. Its size, shape, and location within the uterus help distinguish it from other findings.
Location and Structure
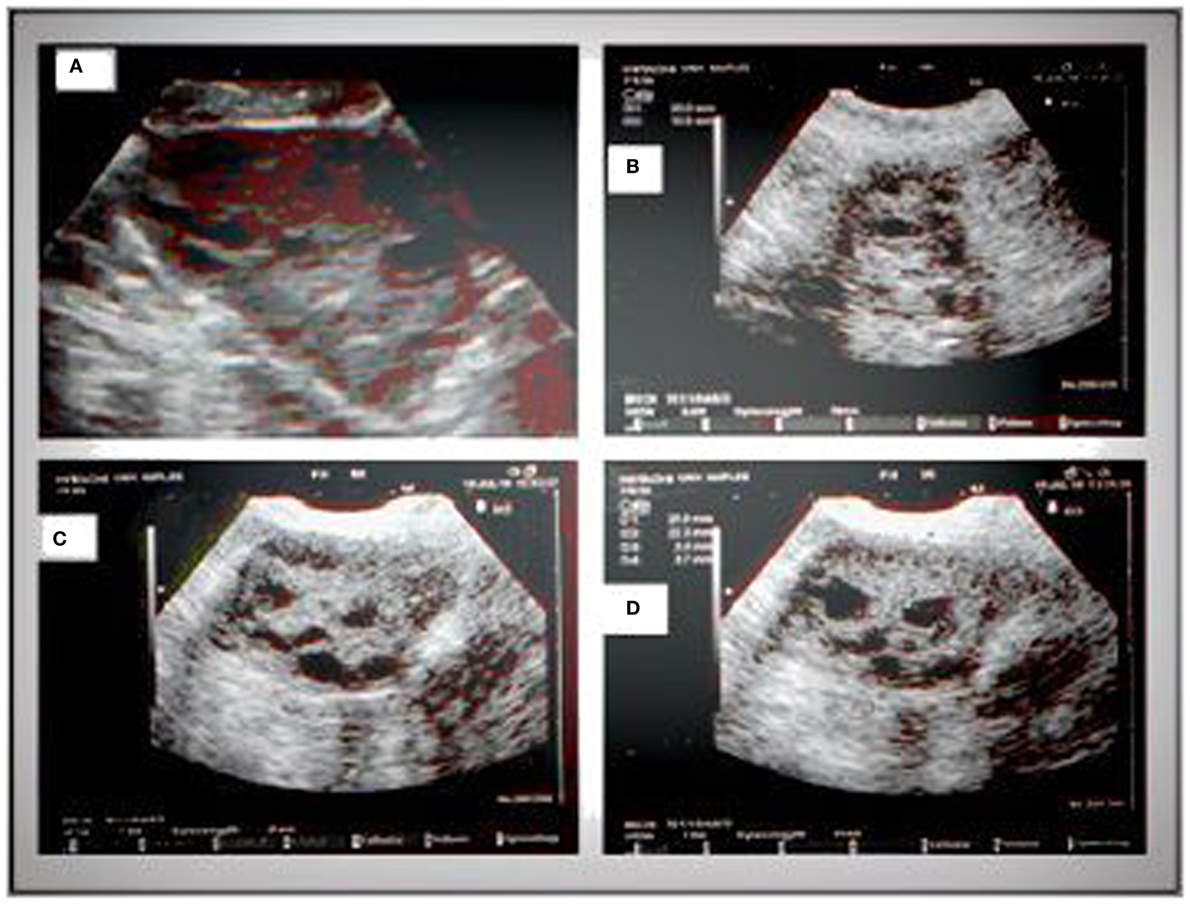
The central echogenic stroma, a prominent feature on ultrasound, occupies a distinct position within the uterus, offering valuable insights into uterine health and function. Understanding its location and structure helps in interpreting ultrasound images and recognizing potential abnormalities.
The central echogenic stroma, also known as the “central echogenic line” or “uterine stripe,” is located within the uterine cavity, specifically in the midline. It appears as a bright, linear echo, often resembling a thin, white line, on ultrasound images. This distinct echogenicity arises from the dense, fibrous connective tissue that constitutes the central echogenic stroma, which is predominantly composed of the following anatomical components:
Components Contributing to Echogenicity
The echogenicity of the central echogenic stroma is attributed to the presence of specific anatomical structures within this region. These components, with their unique properties, contribute to the bright, reflective appearance of the stroma on ultrasound images.
- Endometrial Stroma: The endometrial stroma, a dense layer of connective tissue, plays a crucial role in supporting the endometrium and its cyclical changes. The stroma’s rich vascular network and the presence of collagen fibers contribute to its echogenicity, making it appear brighter than the surrounding tissues on ultrasound.
- Myometrium: The myometrium, the muscular wall of the uterus, lies beneath the endometrium and contributes to the echogenic appearance of the central stroma. The dense muscle fibers and the presence of connective tissue within the myometrium create a reflective surface that enhances echogenicity.
- Blood Vessels: The presence of a network of blood vessels within the central echogenic stroma contributes to its echogenicity. These vessels, carrying blood, create a highly reflective surface, contributing to the bright appearance of the stroma on ultrasound.
Clinical Significance
The presence of a central echogenic stroma (CES) in a fetal ultrasound can be a significant finding, prompting further investigation and careful monitoring. While CES is often a benign finding, it can be associated with certain conditions or situations that may require closer attention. The clinical significance of CES varies depending on several factors, including the gestational age, the presence of other ultrasound abnormalities, and the family history.
CES and Fetal Chromosomal Abnormalities
The presence of CES has been linked to an increased risk of fetal chromosomal abnormalities, particularly trisomy 21 (Down syndrome). Studies have shown that CES is more frequently observed in fetuses with Down syndrome compared to those without. While the exact relationship between CES and chromosomal abnormalities remains unclear, it is thought that CES might be a marker of altered fetal development or a reflection of underlying genetic issues.
- Prevalence: The prevalence of CES in fetuses with Down syndrome is estimated to be significantly higher than in fetuses without Down syndrome. For instance, one study found that CES was present in approximately 30% of fetuses with Down syndrome, compared to only 5% of fetuses without the condition.
- Significance: The presence of CES, especially in combination with other ultrasound abnormalities, may raise concerns about potential chromosomal abnormalities. It can prompt further investigation, such as amniocentesis, to confirm or rule out a diagnosis of Down syndrome or other chromosomal disorders.
CES and Other Fetal Conditions
Besides chromosomal abnormalities, CES has been associated with other fetal conditions, including:
- Fetal heart defects: Some studies have shown a correlation between CES and an increased risk of fetal heart defects. This association may be particularly relevant in cases where CES is present along with other ultrasound findings suggestive of cardiac abnormalities.
- Fetal growth restriction: CES may be observed in fetuses with intrauterine growth restriction (IUGR), a condition where the fetus is not growing at the expected rate. The presence of CES in conjunction with other indicators of IUGR can provide further evidence for this diagnosis.
- Fetal infections: While less common, CES has also been linked to certain fetal infections, such as cytomegalovirus (CMV) infection. The presence of CES in combination with other clinical or ultrasound findings suggestive of fetal infection may warrant further investigation and management.
Causes and Risk Factors
The presence of central echogenic stroma (CES) is often associated with various factors and conditions, which can influence its development and significance. Understanding these causes and risk factors is crucial for providing comprehensive prenatal care and guiding clinical decisions.
Genetic Predisposition
A genetic predisposition plays a significant role in the development of CES. Studies have indicated a correlation between certain genetic mutations and the presence of CES. For instance, mutations in genes responsible for fetal development, such as thetrisomy 21* gene, have been linked to an increased risk of CES. This suggests that certain genetic factors can influence the formation of the fetal brain and potentially contribute to the development of CES.
Management and Monitoring
The management of central echogenic stroma (CES) is primarily focused on monitoring and evaluating the potential risk to the fetus. The presence of CES itself is not a cause for immediate concern, but it serves as a marker that requires further investigation and close observation.
Management Strategies, What is central echogenic stroma
The approach to managing CES depends on various factors, including gestational age, associated symptoms, and the presence of other abnormalities.
Gestational Age
- First Trimester: In the early stages of pregnancy, CES is often observed in isolation. Monitoring with regular ultrasounds is typically recommended to assess fetal growth and development.
- Second Trimester: If CES persists into the second trimester, further investigations may be warranted, especially if other abnormalities are present.
- Third Trimester: The presence of CES in the third trimester may prompt a more thorough evaluation, including fetal echocardiography to assess the heart’s structure and function.
Associated Symptoms
- Absence of Symptoms: If CES is the only anomaly observed and the fetus is otherwise developing normally, regular monitoring is usually sufficient.
- Presence of Symptoms: If CES is accompanied by other fetal abnormalities or if there are concerns about fetal growth or development, further investigations, such as amniocentesis or fetal MRI, may be recommended.
Management Table
The following table Artikels different management strategies based on gestational age and associated symptoms:| Gestational Age | Associated Symptoms | Management Strategy ||—|—|—|| First Trimester | None | Regular ultrasounds to monitor fetal growth and development || Second Trimester | None | Regular ultrasounds, possible fetal echocardiography || Third Trimester | None | Detailed fetal echocardiography, possible amniocentesis or fetal MRI || First Trimester | Present | Further investigation, such as amniocentesis or fetal MRI || Second Trimester | Present | Further investigation, possible fetal echocardiography, amniocentesis or fetal MRI || Third Trimester | Present | Comprehensive fetal evaluation, including fetal echocardiography, amniocentesis, fetal MRI, and genetic counseling |
Future Research and Perspectives: What Is Central Echogenic Stroma
The field of central echogenic stroma (CES) research is continuously evolving, with ongoing efforts to unravel the intricate mechanisms underlying its development and the implications for fetal well-being. Future research holds immense potential to refine our understanding and enhance the management of CES, ultimately improving outcomes for affected pregnancies.
Areas for Further Research
Further research in CES is essential to refine our understanding of its pathogenesis, improve diagnostic accuracy, and develop effective management strategies.
- Unraveling the Molecular Mechanisms: Delving into the molecular pathways involved in CES formation can provide insights into the underlying causes and potentially identify targets for therapeutic interventions. Research focusing on genetic and epigenetic factors, as well as the role of specific proteins and signaling pathways, can shed light on the complex interplay of factors contributing to CES development.
- Improving Diagnostic Accuracy: Developing more accurate and reliable diagnostic tools is crucial for early detection and timely management of CES. This could involve exploring novel imaging techniques, such as advanced ultrasound modalities or magnetic resonance imaging, to improve visualization and characterization of CES. Additionally, research into biomarkers that can differentiate benign from potentially harmful CES could significantly enhance diagnostic accuracy.
- Predicting Long-Term Outcomes: Establishing reliable predictors of long-term outcomes for infants with CES is paramount for informed counseling and management. Research investigating the correlation between CES characteristics, such as size, location, and echogenicity, with long-term developmental outcomes, including neurodevelopmental delays and physical health issues, can provide valuable insights for clinical decision-making.
- Exploring Therapeutic Options: While CES often resolves spontaneously, research exploring potential therapeutic interventions for cases with persistent or severe CES is warranted. This could involve investigating the efficacy of medications, targeted therapies, or even minimally invasive surgical procedures to address underlying causes or mitigate potential complications associated with CES.
Implications of Ongoing Research
Ongoing research in CES holds immense potential to transform our understanding and management of this condition.
- Personalized Management Strategies: By elucidating the diverse factors contributing to CES development, research can pave the way for personalized management strategies tailored to individual patient characteristics. This could involve risk stratification based on specific CES features, genetic predisposition, or other relevant factors, allowing for targeted interventions and improved outcomes.
- Enhanced Counseling and Patient Education: A deeper understanding of CES will empower healthcare professionals to provide more accurate and informative counseling to parents. Clear and comprehensive information about CES, including its potential implications and management options, can alleviate anxiety and foster informed decision-making.
- Improved Fetal Monitoring and Intervention: Research into CES may lead to the development of advanced fetal monitoring techniques that can detect subtle changes associated with CES and predict potential complications. This could enable timely intervention and optimize fetal well-being throughout pregnancy.
Research Study Design
A prospective, longitudinal study investigating the long-term outcomes for patients with CES could provide valuable insights into the natural history of this condition and its impact on long-term health.
- Study Population: The study population should include a large cohort of infants diagnosed with CES during pregnancy, encompassing a diverse range of CES characteristics, such as size, location, and echogenicity.
- Data Collection: Comprehensive data should be collected at multiple time points throughout the pregnancy and postnatally, including detailed ultrasound measurements of CES, maternal and fetal medical history, and relevant genetic information. Longitudinal follow-up assessments should be conducted to evaluate neurodevelopmental milestones, physical health status, and any associated complications.
- Outcome Measures: The study should assess a range of outcomes, including neurodevelopmental milestones (e.g., cognitive function, motor skills, language development), physical health status (e.g., growth, organ function), and any long-term complications associated with CES. This comprehensive approach will provide a comprehensive understanding of the long-term impact of CES on overall health and well-being.
- Statistical Analysis: Statistical analysis should be performed to identify potential correlations between CES characteristics, maternal factors, and long-term outcomes. This will help determine if specific CES features or maternal characteristics are associated with increased risk of adverse outcomes.
Central echogenic stroma is a common finding on ultrasound examinations, particularly during the first trimester of pregnancy. While it often signifies a normal development, it can also be associated with certain conditions, necessitating further investigation and monitoring. Understanding the clinical significance of central echogenic stroma, its potential causes, and appropriate management strategies is essential for ensuring optimal pregnancy outcomes. Ongoing research continues to shed light on this fascinating phenomenon, leading to more accurate diagnoses and effective treatment approaches.
FAQ Section
Is central echogenic stroma always a cause for concern?
No, central echogenic stroma is often a normal finding during pregnancy. However, its presence can sometimes be associated with certain conditions, such as chromosomal abnormalities or placental problems. Therefore, further investigation and monitoring may be necessary in some cases.
What happens if central echogenic stroma is detected during an ultrasound?
The doctor will typically recommend further monitoring and may order additional tests, such as a more detailed ultrasound or genetic testing, depending on the specific circumstances and the presence of any other abnormalities.
Does central echogenic stroma always disappear during pregnancy?
In most cases, central echogenic stroma gradually diminishes as the pregnancy progresses. However, in some cases, it may persist throughout the pregnancy, particularly if it is associated with a specific condition.
Can central echogenic stroma affect the baby’s health?
The presence of central echogenic stroma itself does not necessarily indicate a problem with the baby’s health. However, if it is associated with other abnormalities, it may be a sign of a potential issue. Further evaluation and monitoring are crucial in these cases.






