What is central echogenic stroma in ovary – What is central echogenic stroma in the ovary? This intriguing question delves into the realm of reproductive health, where the intricate workings of the female reproductive system are explored. Central echogenic stroma (CES) is a common finding on ultrasound imaging of the ovaries, and its presence can spark curiosity and sometimes even concern. This structure, often described as a bright, dense area within the ovary, has captured the attention of both clinicians and researchers, leading to a deeper understanding of its potential significance.
CES is a normal component of the ovary, typically located in the center. It appears as a bright, white area on ultrasound due to its dense, fibrous composition. The presence of CES is usually considered benign, meaning it is not cancerous. However, in some cases, CES can be associated with certain ovarian conditions, making it important to understand its characteristics and potential implications.
Introduction to Central Echogenic Stroma
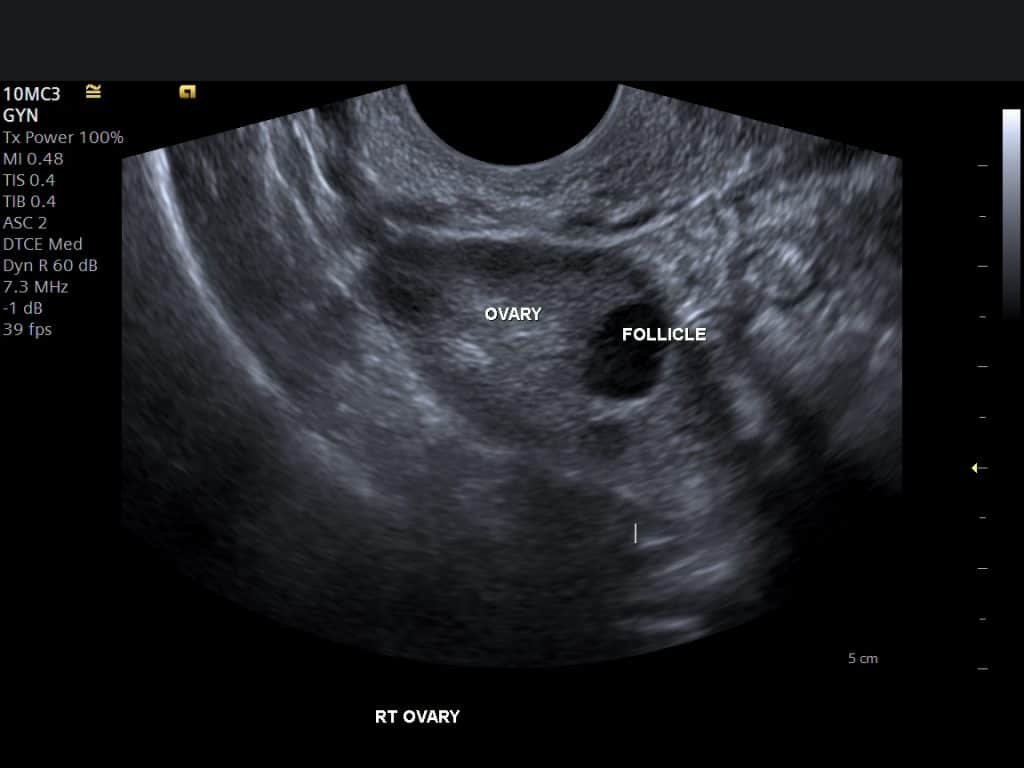
Central echogenic stroma (CES) is a common finding on ultrasound imaging of the ovaries. It refers to a bright, echogenic area located in the center of the ovary, representing the ovarian stroma, the tissue that surrounds the follicles and the egg cells. The ovarian stroma is primarily composed of connective tissue, blood vessels, and smooth muscle fibers.CES is typically a benign finding and does not usually indicate any underlying pathology.
However, in some cases, it can be associated with certain conditions, such as polycystic ovary syndrome (PCOS), ovarian hyperstimulation syndrome (OHSS), and ovarian torsion.
Appearance of CES on Ultrasound Imaging
CES appears as a bright, echogenic area on ultrasound imaging. It is typically well-defined and may be round or oval in shape. The echogenicity of CES can vary depending on the ultrasound machine and the patient’s body habitus. The appearance of CES can be differentiated from other echogenic structures in the ovary, such as follicles, cysts, and tumors. Follicles appear as round, anechoic structures with a thin, echogenic wall.
Cysts are fluid-filled structures that appear anechoic or hypoechoic on ultrasound. Tumors can have a variety of appearances, depending on their type and size.
Prevalence of CES
CES is a common finding on ultrasound imaging of the ovaries. Studies have shown that the prevalence of CES is high, ranging from 50% to 80% in women of reproductive age. The prevalence of CES may vary depending on the population studied and the ultrasound criteria used to define CES.
CES is a common finding on ultrasound imaging of the ovaries, with a prevalence ranging from 50% to 80% in women of reproductive age.
Physiological Significance of CES

The central echogenic stroma (CES) is a distinct feature of the ovary, often observed on ultrasound imaging. While its exact function remains under investigation, there is growing evidence suggesting a significant role in ovarian physiology. This section delves into the potential role of CES in ovarian function, particularly its relationship with follicular development, and how it might vary across different age groups.
CES and Follicular Development
The presence and characteristics of CES have been linked to follicular development and ovarian reserve.
- Increased CES Volume: Studies have indicated a correlation between increased CES volume and a higher number of antral follicles, suggesting a potential association with increased ovarian reserve.
- CES Characteristics: The echogenicity of CES, often described as “hyperechoic,” has been linked to the density of the stromal tissue. Some studies have shown that a more hyperechoic CES may be associated with a higher number of antral follicles and potentially better ovarian response to stimulation during assisted reproductive technologies (ART).
- Follicle Recruitment: While the exact mechanism is not fully understood, CES may play a role in the recruitment and development of follicles. The dense stromal tissue could provide a supportive environment for follicular growth and maturation.
CES in Different Age Groups
The appearance and characteristics of CES can vary across different age groups.
- Younger Women: In younger women with higher ovarian reserve, CES tends to be more prominent and hyperechoic, potentially reflecting a denser stromal tissue.
- Older Women: As women age, the ovarian reserve declines, and CES may become less prominent and less hyperechoic. This could be related to changes in the ovarian stromal tissue associated with aging.
Clinical Implications of CES: What Is Central Echogenic Stroma In Ovary
Central echogenic stroma (CES) is a common finding on ultrasound examinations of the ovaries, and its presence can have a variety of clinical implications. While CES is generally considered a benign finding, its presence can sometimes be associated with specific ovarian conditions and may be a factor in infertility.
Associations with Ovarian Conditions
The presence of CES can be associated with several ovarian conditions, including:
- Polycystic Ovarian Syndrome (PCOS): CES is frequently observed in women with PCOS, often alongside other characteristic features like multiple follicles and ovarian enlargement.
- Ovarian Hyperstimulation Syndrome (OHSS): In women undergoing fertility treatments, CES may be more prominent in those who develop OHSS, a condition characterized by ovarian enlargement and fluid accumulation in the abdomen.
- Ovarian Torsion: While not directly related to CES, the presence of a large, echogenic mass within the ovary, like a large CES, can make it more difficult to diagnose ovarian torsion, a condition where the ovary twists on its blood supply.
CES and Infertility, What is central echogenic stroma in ovary
The role of CES in infertility is not fully understood, but several studies have explored its potential impact.
- Reduced Ovarian Reserve: Some research suggests that CES may be associated with a lower ovarian reserve, which can impact fertility. However, further studies are needed to confirm this association.
- Ovulation Rate: While some studies have shown that CES may be associated with a lower ovulation rate, others have found no significant correlation. More research is needed to clarify this relationship.
Clinical Implications of CES Based on Size, Shape, and Echogenicity
The clinical implications of CES can vary depending on its size, shape, and echogenicity. Here’s a table summarizing potential implications:
| Feature | Potential Implications |
|---|---|
| Large Size | May be associated with PCOS, OHSS, or other ovarian conditions. Could make it more difficult to visualize other ovarian structures. |
| Irregular Shape | May suggest an underlying ovarian condition or be a sign of inflammation or scarring. |
| Hyperechoic | May indicate increased vascularity or fibrosis within the ovary. Could be associated with PCOS or other conditions. |
Diagnostic Considerations
Accurate identification of CES is crucial for proper management and patient counseling. While CES is a common finding, it’s essential to differentiate it from other echogenic structures within the ovary, as these may indicate different conditions requiring distinct approaches.
Differential Diagnoses for CES
A comprehensive understanding of potential differential diagnoses is essential for accurate interpretation of ovarian ultrasound findings. Several conditions can mimic CES, and a careful evaluation is necessary to rule out other possibilities.
- Ovarian Cysts: These are fluid-filled sacs within the ovary. While some cysts may appear echogenic, their characteristics often differ from CES. For example, a hemorrhagic cyst may appear echogenic due to blood content, but it usually demonstrates internal septations or a more complex internal architecture.
- Fibroids: These benign tumors originating from the uterine muscle can occasionally extend into the ovary, appearing as echogenic structures. However, fibroids typically have a more well-defined, rounded shape and may exhibit a characteristic “halo” sign, which is a thin, hypoechoic rim surrounding the echogenic mass.
- Endometriomas: These are cysts filled with blood and tissue from the endometrium, the lining of the uterus. They often appear echogenic due to internal hemorrhage and can be confused with CES, particularly when small. However, endometriomas may demonstrate internal septations or a more complex internal architecture, and their location within the ovary, often adjacent to the uterus, can be helpful in distinguishing them from CES.
- Ovarian Cancer: While rare, ovarian cancer can also present as an echogenic mass. In these cases, the echogenic mass may be larger, more irregular in shape, and may demonstrate signs of invasion into surrounding tissues, such as ascites or enlarged lymph nodes.
- Other Benign Conditions: Other benign conditions, such as ovarian torsion, may also present as echogenic structures. Ovarian torsion, a twisting of the ovary, can lead to blood flow obstruction and subsequent edema, resulting in an echogenic appearance. However, the presence of pain, tenderness, and a lack of normal ovarian flow on Doppler ultrasound can help differentiate ovarian torsion from CES.
Diagnostic Approach for CES
A systematic approach is crucial for accurate diagnosis and management.
- Detailed Ultrasound Evaluation: A comprehensive ultrasound examination, including transvaginal and transabdominal scans, is essential. The size, shape, location, and internal architecture of the echogenic structure should be carefully assessed.
- Doppler Ultrasound: Doppler ultrasound can evaluate blood flow within the echogenic structure. CES typically demonstrates normal vascularity, while other conditions, such as ovarian torsion or some tumors, may show abnormal blood flow patterns.
- Clinical History and Examination: A thorough patient history, including age, menstrual history, and any symptoms, is crucial. Physical examination may reveal tenderness or masses in the pelvic region.
- Follow-up Imaging: Serial ultrasound examinations can monitor the size and appearance of the echogenic structure over time. This can help differentiate CES from other conditions that may grow or change in size.
- Other Tests: In some cases, additional tests, such as a CA-125 blood test or a pelvic MRI, may be recommended to further evaluate the echogenic structure and rule out other possibilities.
Management and Follow-Up
The management of CES is primarily focused on monitoring and reassurance, as the condition is generally benign and does not require specific treatment. The primary goal is to rule out other conditions that may mimic CES and to identify any potential complications.
Ultrasound Monitoring for CES
Ultrasound monitoring plays a crucial role in the management of CES. It allows for the assessment of the size, shape, and echogenicity of the CES, as well as the identification of any changes over time. Regular ultrasound examinations can help to differentiate CES from other ovarian masses, such as cysts, tumors, or endometriomas, and to detect any potential complications, such as torsion or rupture.
Recommended Follow-Up Strategies for Patients with CES
The frequency of follow-up ultrasound examinations for patients with CES depends on several factors, including the patient’s age, symptoms, and the size and characteristics of the CES.
| Patient Characteristics | Recommended Follow-Up |
|---|---|
| Premenopausal women with asymptomatic CES < 3 cm | Annual ultrasound examination |
| Premenopausal women with asymptomatic CES ≥ 3 cm | Every 6 months ultrasound examination |
| Postmenopausal women with asymptomatic CES | Every 3-6 months ultrasound examination |
| Women with symptomatic CES (e.g., pelvic pain, irregular bleeding) | Further evaluation and management based on the specific symptoms |
Research and Future Directions

The understanding of central echogenic stroma (CES) in the ovary is continuously evolving. Ongoing research aims to clarify its exact nature, significance, and clinical implications. Further research is crucial to improve the management of CES and enhance patient care.
Emerging Research Findings
Recent research findings have shed light on various aspects of CES:
- CES and Ovarian Reserve: Studies have explored the potential correlation between CES and ovarian reserve, suggesting that its presence might be associated with reduced ovarian function. However, further investigation is needed to establish a definitive link.
- CES and Ovarian Cancer Risk: Some research suggests a possible association between CES and an increased risk of developing ovarian cancer. However, this link requires further confirmation and investigation.
- CES and Reproductive Outcomes: The impact of CES on reproductive outcomes, such as fertility and pregnancy rates, is an area of ongoing research. Understanding this relationship can guide clinical decision-making.
Areas for Future Research
Several key areas warrant further investigation:
- CES Pathogenesis: The precise mechanisms underlying CES development and its variations remain to be fully elucidated. Research into the cellular and molecular processes involved is crucial.
- CES and Ovarian Function: Further research is needed to clarify the relationship between CES and ovarian function, including its potential impact on ovarian reserve and hormone production.
- CES and Ovarian Cancer: More comprehensive studies are required to determine the potential association between CES and ovarian cancer risk, including identifying potential risk factors and early detection strategies.
- CES and Reproductive Outcomes: Research should focus on understanding the impact of CES on fertility, pregnancy rates, and potential complications during pregnancy.
- CES Management Strategies: Studies investigating the efficacy of different management approaches for CES, including conservative monitoring, surgical intervention, and potential medical therapies, are essential.
Impact of Emerging Technologies
Advances in imaging technologies, such as high-resolution ultrasound and magnetic resonance imaging (MRI), are enhancing the visualization and characterization of CES. These technologies can provide more detailed information about CES morphology and its potential association with other ovarian structures.
“The application of artificial intelligence (AI) in medical imaging holds promise for improving the detection, characterization, and management of CES.”
AI algorithms can analyze large datasets of ultrasound and MRI images, potentially leading to more accurate and objective assessments of CES. This could improve diagnostic accuracy, predict potential complications, and personalize treatment plans.
In conclusion, central echogenic stroma (CES) is a fascinating aspect of ovarian anatomy that has gained significant attention in the field of reproductive health. While typically considered a benign finding, CES can be associated with specific ovarian conditions, highlighting the importance of understanding its characteristics and potential clinical implications. As research continues to unravel the complexities of CES, our understanding of its role in ovarian function and potential impact on fertility is likely to evolve.
By embracing a comprehensive approach that combines clinical expertise, advanced imaging techniques, and ongoing research, we can ensure the best possible care for patients who present with CES.
FAQ Corner
What is the significance of the size of CES?
The size of CES can be a factor in its potential clinical significance. Larger CES may be associated with certain ovarian conditions, such as polycystic ovary syndrome (PCOS). However, it’s important to note that size alone does not always indicate a problem.
Can CES be associated with pain?
While CES is typically a benign finding, some women may experience pelvic pain or discomfort. However, the presence of pain does not necessarily indicate that CES is the cause. Other factors, such as endometriosis or pelvic inflammatory disease, should be considered.
Is CES always visible on ultrasound?
CES may not always be visible on ultrasound, particularly in younger women. The appearance and size of CES can vary depending on factors such as age, hormonal status, and individual variations in ovarian anatomy.





