Does the stroma heal in a cornea transplant? This question delves into the intricate world of corneal transplantation, a procedure that offers hope for restoring vision to those suffering from corneal diseases. The cornea, the transparent outer layer of the eye, is responsible for focusing light onto the retina. The stroma, the middle layer of the cornea, provides structural support and plays a crucial role in maintaining its transparency.
Understanding how the stroma heals after a transplant is essential for successful graft survival and visual recovery.
Corneal transplants involve replacing damaged or diseased corneal tissue with healthy donor tissue. The procedure involves surgically removing the affected portion of the cornea and replacing it with a donor cornea. The success of a corneal transplant depends on several factors, including the type of transplant, the recipient’s immune system, and the ability of the stroma to heal properly.
Understanding the Cornea and Stroma
The cornea is the transparent, dome-shaped outer layer of the eye that plays a crucial role in focusing light onto the retina. It is composed of five distinct layers, each with its own unique structure and function. The stroma, the middle layer of the cornea, is the thickest and most important layer, accounting for approximately 90% of the cornea’s total thickness.
The stroma is responsible for maintaining the cornea’s structural integrity and transparency. It is a highly organized and densely packed matrix of collagen fibrils embedded in a hydrated proteoglycan gel. This unique structure allows the cornea to transmit light effectively, ensuring clear vision.
Cellular Components of the Stroma
The stroma is primarily composed of collagen fibrils, which are arranged in a highly organized and parallel fashion. These fibrils are responsible for the cornea’s strength and resilience. In addition to collagen, the stroma also contains other important cellular components, including:
- Keratocytes: These are the primary cells of the stroma. They are responsible for synthesizing and maintaining the collagen fibrils and other components of the extracellular matrix. Keratocytes are quiescent cells that are activated during wound healing.
- Fibroblasts: These are similar to keratocytes and are involved in wound healing and scar formation.
- Endothelial cells: These cells line the inner surface of the cornea and play a role in maintaining corneal hydration and transparency.
Cornea Transplant Procedures

A cornea transplant, also known as corneal transplantation, is a surgical procedure that replaces a damaged or diseased cornea with a healthy one from a donor. This procedure is a highly effective treatment for a range of corneal conditions, including keratoconus, corneal dystrophies, and scarring from injuries or infections.
Types of Cornea Transplants
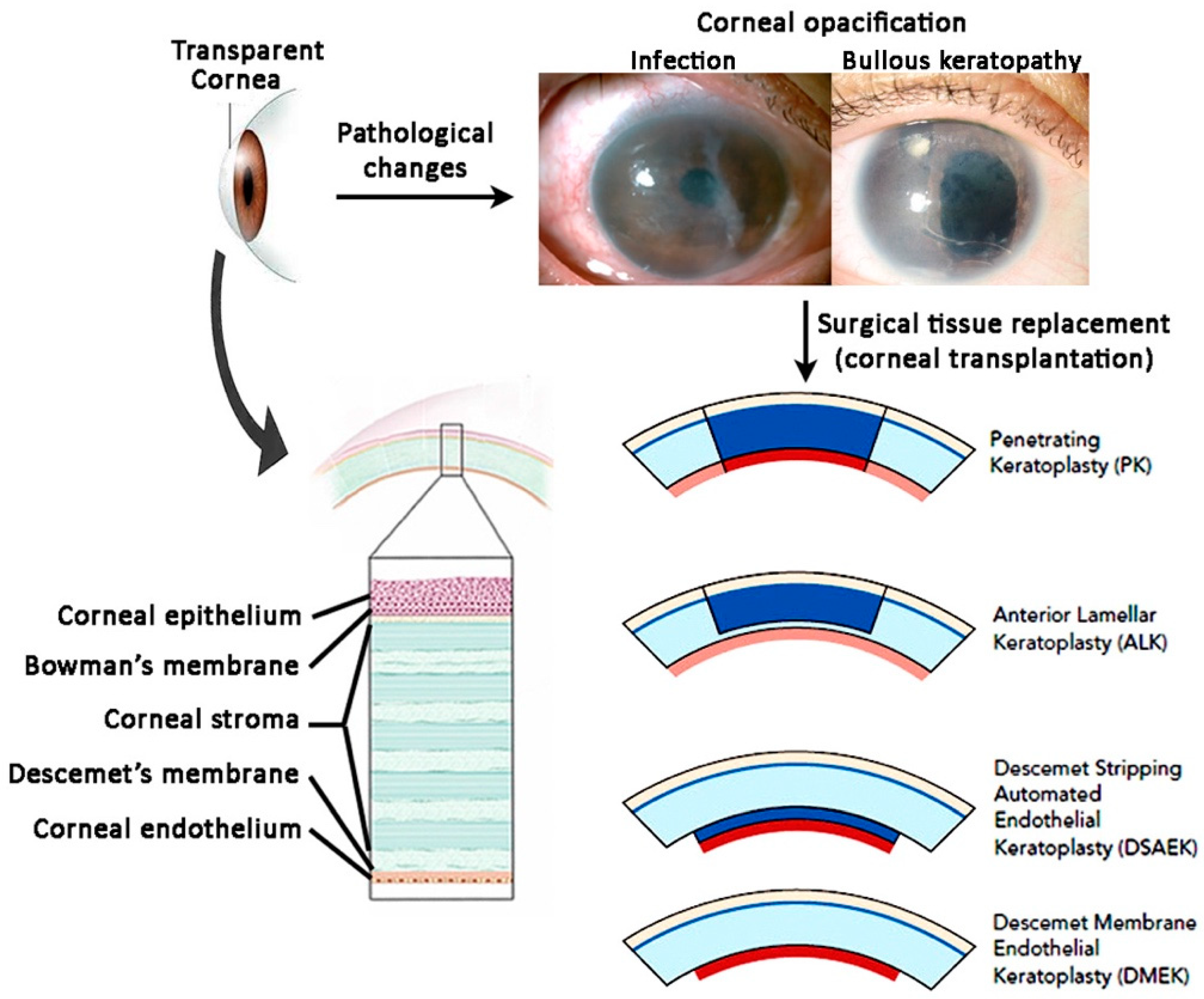
The type of cornea transplant performed depends on the extent and nature of the corneal damage.
- Penetrating Keratoplasty (PK): This is the most common type of corneal transplant, involving the replacement of the full thickness of the cornea, from the outer surface (epithelium) to the inner surface (endothelium). It is used for conditions affecting all layers of the cornea.
- Lamellar Keratoplasty (LK): This procedure involves replacing only a partial thickness of the cornea. There are several types of LK, including:
- Deep Lamellar Keratoplasty (DALK): Replaces the deeper layers of the cornea, leaving the endothelium intact. It is used for conditions affecting the stroma and Bowman’s layer.
- Endothelial Keratoplasty (EK): Replaces only the endothelium, the innermost layer of the cornea. It is used for conditions affecting the endothelium, such as Fuchs’ endothelial dystrophy.
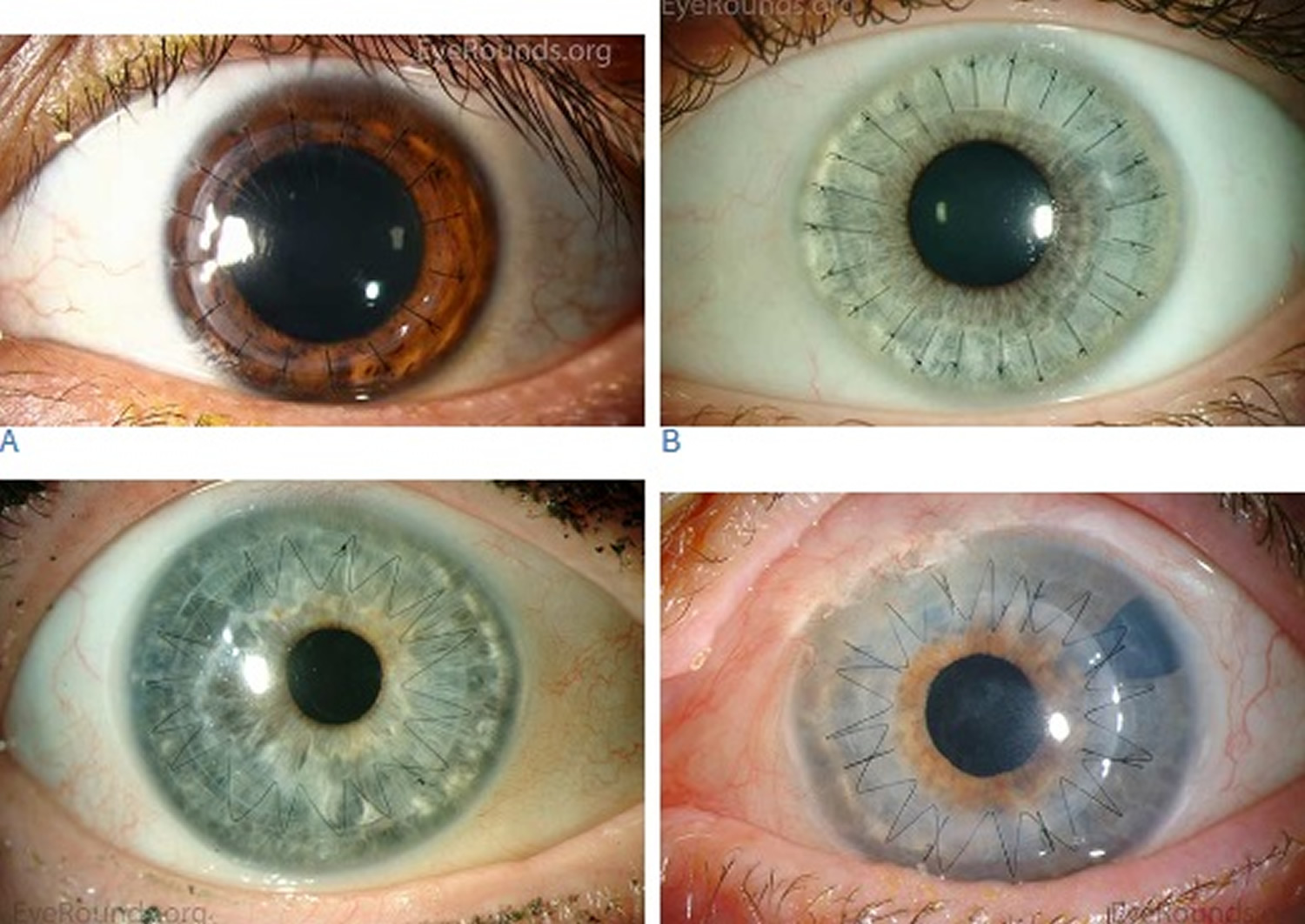
Surgical Procedure for a Cornea Transplant
The surgical procedure for a corneal transplant is typically performed under local anesthesia, meaning the eye is numbed, but the patient remains awake. The procedure involves the following steps:
- Preparation: The surgeon will first clean and sterilize the eye. They will then use a special instrument to cut a circular flap in the outer layer of the cornea (epithelium). This flap is folded back to expose the underlying cornea.
- Donor Cornea Preparation: The donor cornea, which has been carefully screened and preserved, is then prepared. It is cut to the appropriate size and shape to fit the recipient’s eye.
- Donor Cornea Placement: The surgeon carefully removes the diseased portion of the recipient’s cornea and replaces it with the donor cornea. The flap is then folded back into place and secured with sutures.
- Sutures: The sutures are usually placed on the outer surface of the cornea and are typically removed several months after surgery.
Post-Operative Care
Following a cornea transplant, it is crucial to follow the surgeon’s instructions for post-operative care. This typically includes:
- Eye Drops: Regular use of prescribed eye drops to prevent infection, reduce inflammation, and promote healing.
- Protective Shield: Wearing a protective shield over the eye at night to prevent accidental injury.
- Follow-up Appointments: Regular follow-up appointments with the surgeon to monitor the healing process and ensure the transplant is successful.
- Lifestyle Modifications: Avoiding activities that could put stress on the eye, such as rubbing the eye, swimming, and contact sports.
Healing After a Corneal Transplant
The healing process following a corneal transplant is complex and involves a delicate interplay between the recipient’s immune system and the transplanted corneal tissue. This process aims to integrate the new corneal tissue into the recipient’s eye while maintaining its transparency and visual function.
Wound Healing in the Cornea
After the corneal transplant surgery, the recipient’s body initiates a wound healing response to repair the surgical incisions and integrate the transplanted tissue. This process involves several stages, including inflammation, cell proliferation, and tissue remodeling.The initial phase involves inflammation, characterized by the influx of immune cells to the surgical site. These cells, such as neutrophils and macrophages, help clear debris and foreign materials, contributing to the initial healing process.
Subsequently, cells like fibroblasts and epithelial cells proliferate and migrate to the wound area, promoting tissue repair and closure. The final stage involves tissue remodeling, where the newly formed tissue is organized and strengthened, ultimately leading to the integration of the transplanted cornea.
Stroma Healing in a Corneal Transplant
The stroma, the middle layer of the cornea, plays a crucial role in maintaining the cornea’s shape and clarity. In a corneal transplant, the damaged stroma is replaced with a healthy donor stroma. The healing process of the stroma is essential for the success of the transplant, as it determines the clarity of vision and the long-term stability of the graft.
Factors Influencing Stroma Healing
Several factors influence the healing of the stroma after a corneal transplant. These factors include:
- Age of the recipient: Younger recipients tend to have a faster healing process compared to older recipients.
- Health of the recipient: Underlying medical conditions, such as diabetes or autoimmune diseases, can affect the healing process and increase the risk of rejection.
- Type of corneal transplant: The type of corneal transplant performed influences the healing process and the potential for rejection.
- Surgical technique: The surgical technique used during the transplant procedure can affect the healing process and the outcome of the transplant.
- Post-operative care: Proper post-operative care, including medication and follow-up appointments, is crucial for optimal healing and reducing the risk of rejection.
Comparison of Stroma Healing in Different Transplant Types, Does the stroma heal in a cornea transplant
The healing process of the stroma varies depending on the type of corneal transplant performed.
- Penetrating keratoplasty (PK): This type of transplant involves replacing the entire thickness of the cornea, including the stroma. Healing in PK involves the integration of the donor stroma with the recipient’s stroma. The healing process can take several months to complete, and the risk of rejection is higher compared to other types of corneal transplants.
- Lamellar keratoplasty (LK): This type of transplant involves replacing only a portion of the cornea, typically the stroma. Healing in LK is generally faster than in PK, and the risk of rejection is lower. There are different types of LK procedures, including DMEK (Descemet’s membrane endothelial keratoplasty) and DSAEK (Descemet’s stripping automated endothelial keratoplasty). DMEK involves transplanting only the Descemet’s membrane and the endothelial cells, while DSAEK involves transplanting a portion of the Descemet’s membrane and the endothelial cells along with a thin layer of the stroma.
Rejection and its Impact on Stroma Healing
Rejection is a major complication that can occur after a corneal transplant. It is an immune response by the recipient’s body against the donor tissue. Rejection can affect the healing process of the stroma and lead to graft failure.
- Signs of rejection: The signs of rejection include decreased vision, redness, pain, and increased sensitivity to light.
- Treatment of rejection: Treatment of rejection involves using immunosuppressive medications to suppress the immune response and prevent further damage to the graft.
Techniques for Enhancing Stroma Healing
After a corneal transplant, the body’s natural healing process begins, but it can be slow and sometimes incomplete. Techniques to enhance stroma healing aim to accelerate the process and improve the long-term success of the transplant. These techniques focus on minimizing inflammation, promoting cell growth, and supporting the integration of the donor cornea with the recipient’s tissue.
Medications and Other Treatments
Medications and other treatments play a significant role in promoting stroma healing after a corneal transplant. They are administered to manage inflammation, prevent rejection, and support the integration of the donor cornea.
- Anti-inflammatory medications: These medications help reduce inflammation and swelling in the eye, which can hinder healing. Common examples include corticosteroids, such as prednisolone, and non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen.
- Immunosuppressant medications: These medications suppress the body’s immune system to prevent it from rejecting the donor cornea. Examples include cyclosporine, tacrolimus, and azathioprine.
- Antibiotics: Antibiotics are prescribed to prevent and treat infections that can delay healing.
- Artificial tears: These lubricating drops help keep the eye moist and prevent dryness, which can irritate the healing cornea.
- Eye patches: Eye patches are often used after surgery to protect the eye and promote healing.
Stem Cell Therapy
Stem cell therapy holds promise for enhancing stroma healing after corneal transplants. Stem cells are undifferentiated cells that have the potential to develop into various cell types, including corneal cells.
- Limbal stem cell transplantation: This procedure involves transplanting stem cells from the limbus, the junction between the cornea and conjunctiva, to the damaged cornea. Limbal stem cells can regenerate corneal epithelial cells, which are essential for maintaining the corneal surface and protecting the eye.
- Amniotic membrane transplantation: Amniotic membrane, a thin membrane that surrounds the fetus during pregnancy, contains stem cells and growth factors that can promote corneal healing. Amniotic membrane transplantation has been used to treat various corneal diseases, including corneal ulcers and scarring.
Comparison of Approaches
The table below compares different approaches to enhance stroma healing after a corneal transplant:
| Approach | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| Medications | Reduce inflammation, prevent rejection, support integration | Widely available, relatively affordable, proven efficacy | Side effects, potential for long-term complications, may not be effective for all patients |
| Stem cell therapy | Regenerate corneal cells, promote healing | Potential for long-term corneal health, may be effective for patients with severe corneal damage | Relatively new, not widely available, high cost, ongoing research needed |
Long-Term Outcomes and Considerations: Does The Stroma Heal In A Cornea Transplant
Corneal transplantation, a surgical procedure that replaces damaged or diseased corneal tissue with healthy donor tissue, offers the potential for significant vision improvement and restoration. The long-term success of a corneal transplant depends on various factors, including the underlying cause of corneal disease, the patient’s overall health, and the quality of the donor tissue. The healing of the stroma, the middle layer of the cornea, plays a crucial role in the long-term outcome of the procedure.
Regular Follow-Up Appointments
Regular follow-up appointments after a corneal transplant are essential for monitoring the healing process and detecting any complications. These appointments typically involve a comprehensive eye examination, including visual acuity testing, slit-lamp examination, and corneal topography.
- During these appointments, the ophthalmologist will assess the graft’s clarity, the presence of any inflammation or rejection, and the overall health of the cornea.
- Early detection and treatment of complications can significantly improve the long-term success of the transplant.
Vision Improvement and Graft Survival
The primary goal of corneal transplantation is to improve vision. The success of vision improvement varies depending on the underlying corneal disease and the overall health of the patient.
- In some cases, patients may experience a significant improvement in vision, achieving 20/20 or better visual acuity.
- In other cases, vision improvement may be more modest, but still provide a significant improvement in quality of life.
Graft survival is another important long-term outcome. The success of a corneal transplant is measured by the duration of time the transplanted tissue remains clear and functional.
- The majority of corneal transplants are successful, with the graft remaining clear and functional for many years.
- However, some grafts may fail due to rejection, infection, or other complications.
The healing of the stroma after a cornea transplant is a complex process influenced by various factors. Understanding these factors and employing strategies to enhance healing is crucial for optimal outcomes. While complications can arise, advancements in surgical techniques and post-operative care have significantly improved the success rates of corneal transplantation. With continued research and innovation, we can expect even better long-term results, offering hope for a brighter future for individuals seeking corneal transplantation.
Questions and Answers
What are the different types of cornea transplants?
There are several types of cornea transplants, including penetrating keratoplasty (PKP), which involves replacing the entire cornea, and lamellar keratoplasty, which involves replacing only a portion of the cornea. The type of transplant depends on the specific condition being treated.
How long does it take for the stroma to heal after a cornea transplant?
The healing process varies depending on the individual and the type of transplant. It can take several months for the stroma to fully heal and for vision to stabilize. Regular follow-up appointments with an ophthalmologist are crucial to monitor healing and address any complications.
What are the potential complications of a cornea transplant?
Potential complications of a cornea transplant include infection, rejection, and graft failure. Early detection and treatment of complications are essential for preserving graft survival and maintaining vision.
What are the long-term outcomes of a cornea transplant?
Long-term outcomes of a cornea transplant vary depending on individual factors. Many individuals experience significant vision improvement, while others may have persistent vision problems. Regular follow-up care is essential for long-term graft survival and visual stability.






