How does corneal stroma regeneration work? Imagine a window to the world, a delicate film that allows light to enter your eyes and create the vibrant tapestry of vision. This is the cornea, and its central layer, the stroma, is a marvel of intricate structure and function. But what happens when this vital layer is damaged, clouding your vision and threatening your sight?
The quest for corneal stroma regeneration has captivated scientists and doctors, seeking to restore the clarity and brilliance of sight.
The corneal stroma, a dense network of collagen fibers, is the cornerstone of the cornea’s strength and transparency. It plays a vital role in refracting light, ensuring sharp vision. However, injuries, diseases, and even aging can compromise its integrity, leading to vision impairment. Corneal transplantation, a complex procedure involving the surgical replacement of the damaged cornea, has been the gold standard for treatment.
But advancements in stem cell therapy, artificial corneal implants, and bioengineering offer promising new avenues for restoring corneal function.
Introduction to Corneal Stroma
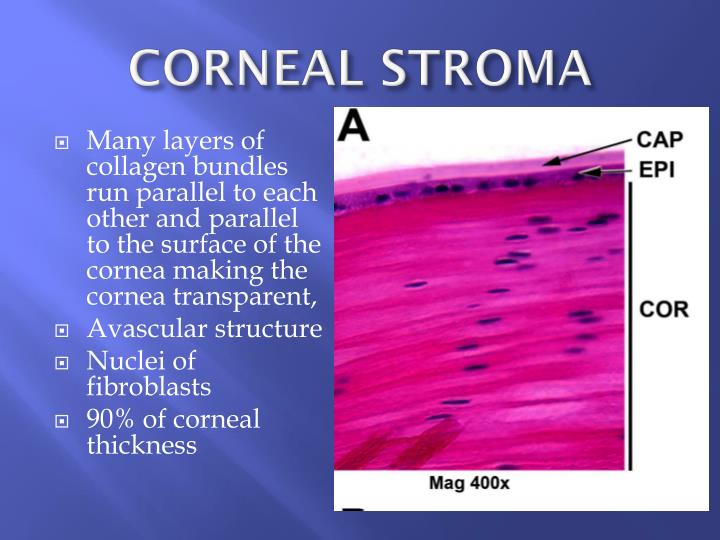
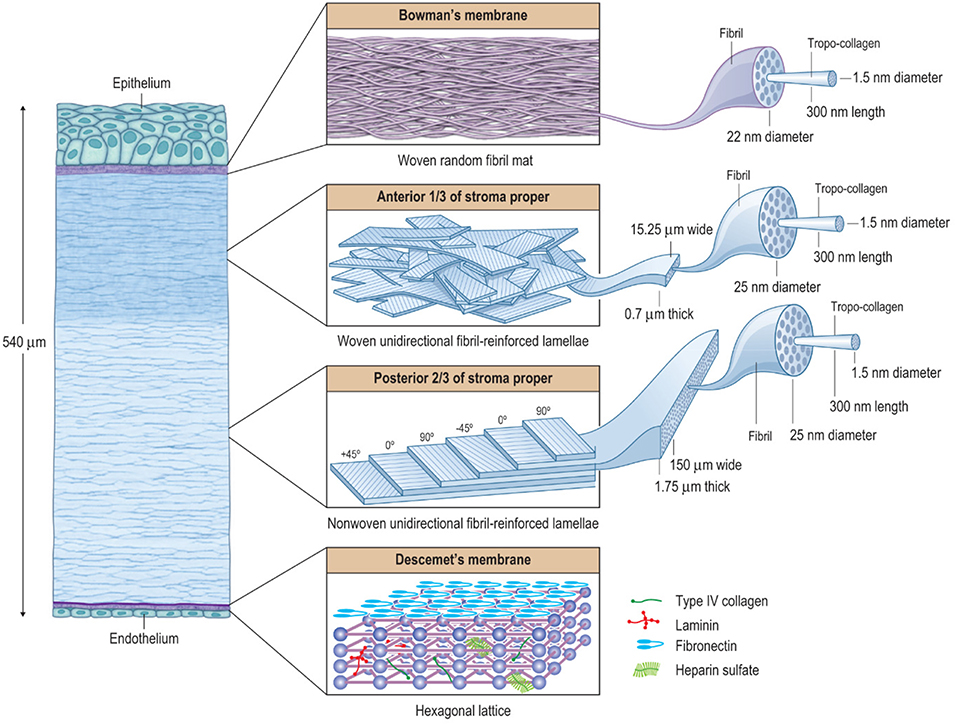
The corneal stroma is the central and thickest layer of the cornea, the transparent outer layer of the eye that plays a crucial role in focusing light onto the retina. It is responsible for maintaining the cornea’s structural integrity and optical clarity, both of which are essential for sharp vision. The corneal stroma is primarily composed of highly organized collagen fibrils embedded in a proteoglycan matrix.
These collagen fibrils are arranged in a parallel, tightly packed, and regularly spaced manner, resembling a stacked, interwoven lattice. This unique arrangement allows for the cornea’s transparency, as light passes through the stroma with minimal scattering.
Importance of Corneal Stroma in Maintaining Vision
The corneal stroma plays a vital role in maintaining clear vision by:
- Providing Structural Support: The stroma’s robust collagen framework gives the cornea its shape and rigidity, preventing it from bulging or collapsing. This structural integrity is crucial for maintaining the cornea’s refractive power, which allows light to focus properly on the retina.
- Ensuring Transparency: The highly organized collagen fibrils and the proteoglycan matrix contribute to the cornea’s transparency, allowing light to pass through with minimal scattering. This is essential for clear vision.
- Maintaining Corneal Hydration: The proteoglycans in the stroma attract and retain water, contributing to the cornea’s hydration. This hydration is essential for maintaining the cornea’s refractive index and transparency.
Challenges Associated with Corneal Stroma Damage
Damage to the corneal stroma can significantly impair vision, leading to various complications. These complications include:
- Corneal Scarring: Injury or infection can damage the stroma, leading to the formation of scar tissue. Scar tissue is opaque, hindering light transmission and causing blurred vision.
- Corneal Edema: Damage to the stroma can disrupt the balance of water in the cornea, leading to corneal edema (swelling). This can distort the cornea’s shape, causing blurred vision and discomfort.
- Corneal Thinning: Damage to the stroma can weaken the cornea, leading to thinning. This can compromise the cornea’s structural integrity, increasing the risk of corneal rupture and vision loss.
Current Methods for Corneal Stroma Regeneration
The cornea, the transparent front part of the eye, plays a crucial role in focusing light onto the retina. Damage to the corneal stroma, the middle layer of the cornea, can lead to vision impairment and blindness. Thankfully, various methods are being explored to regenerate the corneal stroma and restore vision. These methods offer hope for patients with corneal stromal diseases, providing alternative solutions to traditional corneal transplantation.
Corneal Transplantation
Corneal transplantation, also known as keratoplasty, is the gold standard for treating severe corneal stromal diseases. It involves surgically replacing the damaged cornea with a healthy donor cornea. This procedure is effective in restoring vision, but it has limitations.
- Advantages:
- Proven efficacy in restoring vision.
- Relatively high success rate.
- Widely available in many countries.
- Disadvantages:
- Donor cornea availability can be limited.
- Risk of rejection by the recipient’s immune system.
- Surgical procedure carries risks and potential complications.
- Requires careful post-operative management and lifelong immunosuppression.
Artificial Corneal Implants
Artificial corneal implants are biocompatible materials designed to replace the damaged corneal stroma. These implants offer a potential solution for patients who are not suitable for corneal transplantation or who lack access to donor corneas.
- Advantages:
- No need for donor tissue, eliminating the risk of rejection.
- Can be implanted using minimally invasive procedures.
- Potential for personalized customization.
- Disadvantages:
- Still in the early stages of development and clinical trials.
- Long-term efficacy and safety are yet to be fully established.
- Costly and may not be widely accessible.
Stem Cell-Based Therapies
Stem cell-based therapies hold immense promise for corneal stromal regeneration. These therapies utilize the regenerative potential of stem cells to repair damaged corneal tissue.
- Advantages:
- Potential for generating new corneal cells and tissues.
- May reduce the risk of rejection compared to donor corneas.
- Can be customized to the individual patient’s needs.
- Disadvantages:
- Still in the experimental phase and requires further research.
- Challenges in controlling stem cell differentiation and integration into the cornea.
- Potential ethical concerns regarding stem cell sourcing and manipulation.
Cellular Mechanisms of Corneal Stroma Regeneration
The corneal stroma, the transparent, collagen-rich layer of the cornea, possesses a remarkable ability to regenerate following injury. This regenerative process involves a complex interplay of various cell types, signaling pathways, and extracellular matrix components.
Role of Cell Types
The primary cell types involved in corneal stroma regeneration are keratocytes, fibroblasts, and endothelial cells.
- Keratocytes, the resident cells of the corneal stroma, are responsible for maintaining the structural integrity of the stroma. Following injury, keratocytes undergo a process called transdifferentiation, transforming into myofibroblasts, which play a crucial role in wound healing. Myofibroblasts synthesize and deposit extracellular matrix components, including collagen, which are essential for the formation of a new stromal layer.
- Fibroblasts, which are found in the conjunctiva and limbus, can also contribute to corneal stroma regeneration. These cells migrate into the wound site and differentiate into myofibroblasts, aiding in the synthesis and deposition of extracellular matrix components.
- Endothelial cells, which line the inner surface of the cornea, are responsible for maintaining the transparency of the cornea by regulating fluid balance. They also play a role in corneal stromal regeneration by secreting growth factors that stimulate the proliferation and differentiation of other cell types involved in the process.
Signaling Pathways
Several signaling pathways are involved in regulating corneal stroma regeneration. These pathways orchestrate the complex interplay of cell types, growth factors, and extracellular matrix components.
- Wnt pathway: The Wnt pathway is a key regulator of cell proliferation, differentiation, and tissue regeneration. Activation of the Wnt pathway promotes the proliferation and differentiation of keratocytes and fibroblasts, contributing to the formation of new stromal tissue.
- TGF-β pathway: The TGF-β pathway plays a crucial role in wound healing and tissue regeneration. TGF-β signaling promotes the differentiation of fibroblasts into myofibroblasts, stimulates the production of extracellular matrix components, and inhibits the inflammatory response, all of which are essential for corneal stroma regeneration.
Extracellular Matrix Components
The extracellular matrix (ECM) provides structural support to the corneal stroma and plays a vital role in regulating cell behavior.
- Collagen: Collagen is the primary structural component of the corneal stroma, providing tensile strength and transparency. During regeneration, collagen fibers are deposited in a highly organized manner, mimicking the structure of the original stroma.
- Proteoglycans: Proteoglycans are complex molecules that bind to collagen and other ECM components, contributing to the structural integrity and hydration of the corneal stroma. They also play a role in regulating cell adhesion and migration.
- Growth factors: Growth factors, such as fibroblast growth factor (FGF) and epidermal growth factor (EGF), are embedded within the ECM and play a crucial role in stimulating cell proliferation, differentiation, and migration.
Factors Influencing Corneal Stroma Regeneration
The corneal stroma’s remarkable regenerative capacity is influenced by a complex interplay of factors, both intrinsic and extrinsic. Understanding these factors is crucial for optimizing corneal healing and developing effective therapeutic strategies.
Factors Influencing Corneal Stroma Regeneration, How does corneal stroma regeneration
Several factors can either promote or hinder corneal stroma regeneration. These factors can be broadly classified as positive or negative influences.
| Factor | Influence | Explanation |
|---|---|---|
| Age | Negative | As individuals age, their corneal stromal cells exhibit reduced proliferative potential and a slower rate of collagen synthesis. This decline in cellular activity can impair the regeneration process. |
| Underlying health conditions | Negative | Conditions like diabetes, autoimmune diseases, and chronic inflammation can disrupt corneal stromal regeneration. These conditions can compromise cellular function, impair blood supply, and create an unfavorable environment for healing. |
| Severity of injury | Negative | The extent of damage to the corneal stroma significantly impacts regeneration. Extensive injury, such as deep corneal ulcers or penetrating wounds, often leads to more complex healing processes and potentially scar formation. |
| Nutritional status | Positive | Adequate nutrition, particularly a balanced intake of protein, vitamins, and minerals, is essential for supporting corneal stromal regeneration. These nutrients provide the building blocks for new cells and collagen, promoting healing and tissue repair. |
Emerging Technologies for Corneal Stroma Regeneration
The quest for restoring sight to those afflicted by corneal blindness has led to the development of innovative technologies that hold the promise of revolutionizing corneal stroma regeneration. These technologies leverage the principles of bioengineering, tissue engineering, and nanotechnology to create novel solutions for restoring corneal function and vision.
3D Bioprinting of Corneal Tissue
D bioprinting, also known as biofabrication, offers a promising avenue for generating functional corneal tissue. This technology involves the layer-by-layer deposition of biomaterials, cells, and growth factors in a precise 3D pattern, mimicking the intricate structure of the native corneal stroma. The bioprinted constructs can be customized to address specific patient needs, potentially leading to personalized corneal regeneration.
- Bioink Composition: Bioinks used in corneal bioprinting typically consist of biocompatible materials such as hydrogels, collagen, and fibrin, which provide structural support and promote cell adhesion and growth.
- Cell Sources: Various cell sources, including corneal stromal cells, stem cells, and fibroblasts, can be incorporated into the bioink to generate functional corneal tissue.
- Scaffold Design: The design of the 3D scaffold is crucial for replicating the intricate structure and function of the corneal stroma. This involves creating a porous, biocompatible scaffold that facilitates cell migration, proliferation, and differentiation.
Gene Editing Techniques
Gene editing technologies, such as CRISPR-Cas9, offer a powerful tool for modifying corneal cells to enhance their regenerative potential. By precisely targeting and modifying specific genes, these techniques can address genetic defects that contribute to corneal diseases, such as keratoconus and Fuchs’ endothelial dystrophy.
- Gene Correction: Gene editing can be used to correct mutations in genes responsible for corneal stromal defects, restoring normal function and preventing disease progression.
- Enhanced Regeneration: Gene editing can be employed to enhance the regenerative capacity of corneal cells by modifying genes that regulate cell proliferation, differentiation, and extracellular matrix production.
- Immunomodulation: Gene editing can be used to modify immune responses to corneal grafts, reducing the risk of rejection and improving graft survival.
Nanomaterials for Wound Healing
Nanomaterials possess unique properties that make them ideal for promoting corneal wound healing. These materials can enhance cell adhesion, proliferation, and differentiation, as well as modulate inflammation and infection.
- Nanoparticles: Nanoparticles can be engineered to deliver growth factors, antibiotics, or other therapeutic agents directly to the corneal wound site, promoting healing and preventing infection.
- Nanofibers: Nanofibers can be used to create biocompatible scaffolds that mimic the extracellular matrix of the corneal stroma, providing structural support and guiding cell migration and regeneration.
- Nanocoatings: Nanocoatings can be applied to corneal implants or surgical tools to reduce inflammation, improve biocompatibility, and enhance wound healing.
Clinical Applications and Future Directions

The promise of corneal stroma regeneration lies in its potential to revolutionize the treatment of corneal diseases, offering hope for patients facing vision loss or blindness. This section explores the clinical applications of these technologies, outlining how they can address unmet needs in corneal disease management and highlighting the future directions of this exciting field.
Clinical Trial Design
A well-designed clinical trial is crucial for evaluating the effectiveness and safety of new corneal stroma regeneration therapies. The trial should be structured to address specific research questions and objectives, ensuring robust data collection and analysis. The following is an example of a clinical trial design for evaluating a new corneal stroma regeneration therapy:
Objective
To assess the efficacy and safety of a novel bioengineered corneal stroma graft in restoring corneal transparency and visual acuity in patients with corneal opacity.
Study Design
A prospective, randomized, controlled, double-blind clinical trial.
Participants
Patients diagnosed with corneal opacity, aged 18-70 years, with stable vision and no other ocular conditions that could interfere with the study.
Interventions
Intervention Group
Patients will receive a bioengineered corneal stroma graft.
Control Group
Patients will receive a standard corneal transplant.
Outcomes
Primary Outcome
Corneal transparency assessed using a standardized grading system.
Secondary Outcomes
Visual acuity, corneal thickness, and safety measures (e.g., graft rejection, infection).
Data Analysis
Statistical analysis will be performed to compare the outcomes between the intervention and control groups.
Ethical Considerations
The trial will adhere to all ethical guidelines and regulations, including informed consent and patient confidentiality.
Addressing Unmet Needs in Corneal Disease Management
Corneal diseases, including keratoconus, corneal dystrophies, and corneal ulcers, pose significant challenges for ophthalmologists and patients alike. Current treatment options often involve invasive procedures, have limited efficacy, or carry the risk of complications. Corneal stroma regeneration technologies hold the potential to address these unmet needs, offering:* Less Invasive Treatment Options: Regenerative therapies can potentially replace or repair damaged corneal stroma, minimizing the need for invasive surgical procedures.
Improved Efficacy
Bioengineered corneal stroma grafts can potentially achieve better outcomes than traditional corneal transplants, leading to improved visual acuity and a higher chance of graft survival.
Reduced Complications
Regenerative therapies can potentially reduce the risk of complications associated with corneal transplants, such as graft rejection, infection, and astigmatism.
Future Directions of Corneal Stroma Regeneration Research
The field of corneal stroma regeneration is rapidly evolving, with ongoing research focusing on:* Developing Novel Biomaterials: Scientists are exploring new biomaterials that mimic the structure and function of the native corneal stroma, enhancing biocompatibility and promoting tissue integration.
Optimizing Cell Therapies
Research is underway to develop cell-based therapies that can regenerate corneal stroma, including the use of stem cells, fibroblasts, and keratocytes.
Improving Delivery Systems
Researchers are investigating innovative delivery systems for corneal stroma regeneration therapies, such as biocompatible hydrogels, microfluidic devices, and nanoparticles.
Personalized Medicine
The future of corneal stroma regeneration lies in tailoring treatments to individual patients, using genetic and biomechanical information to optimize treatment outcomes.
The journey to restore corneal stroma regeneration is an ongoing saga of scientific exploration and technological innovation. As we delve deeper into the intricate mechanisms of corneal healing, we unlock new possibilities for restoring sight and improving the lives of millions affected by corneal diseases. The future of corneal regeneration holds the promise of personalized therapies, tailored to individual needs, and the potential to overcome the limitations of traditional treatments.
With each breakthrough, we move closer to a world where clear vision is a reality for all.
Essential Questionnaire: How Does Corneal Stroma Regeneration
What are the most common causes of corneal stroma damage?
Common causes of corneal stroma damage include injuries, infections, and degenerative diseases like keratoconus.
How long does it take for corneal stroma regeneration to occur?
The time it takes for corneal stroma regeneration varies depending on the severity of the damage, the individual’s health, and the treatment methods used. Some regeneration may occur naturally, while others require interventions like stem cell therapy.
What are the potential risks associated with corneal stroma regeneration therapies?
As with any medical procedure, corneal stroma regeneration therapies can carry potential risks, including infection, inflammation, and rejection of the transplanted tissue or implant. The specific risks will vary depending on the chosen method and the individual’s health.






