How does smoking affect your stroma and alveolar sacs – How smoking affects your stroma and alveolar sacs sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. Our lungs, the silent heroes of our respiratory system, are intricately designed to fuel our bodies with life-giving oxygen. But what happens when the very air we breathe turns into a silent assassin?
The answer lies in the devastating impact of cigarette smoke on the delicate structures of our lungs, specifically the stroma and alveolar sacs.
Imagine a delicate network of connective tissue, the stroma, providing the framework for the intricate tapestry of your lungs. This vital structure, responsible for the lungs’ ability to expand and contract, is relentlessly attacked by the toxic cocktail of chemicals found in cigarette smoke. This assault triggers inflammation and fibrosis, scarring the stroma and hindering its ability to function properly.
The Respiratory System
The respiratory system is a vital organ system responsible for taking in oxygen and expelling carbon dioxide, essential processes for sustaining life. It comprises a network of organs, including the nose, pharynx, larynx, trachea, bronchi, and lungs, all working in concert to facilitate gas exchange.
Structure and Function
The respiratory system can be broadly divided into two parts: the upper respiratory tract and the lower respiratory tract. The upper respiratory tract, consisting of the nose, pharynx, and larynx, filters, warms, and humidifies inhaled air. The lower respiratory tract, including the trachea, bronchi, and lungs, is responsible for the actual gas exchange. The trachea, or windpipe, is a tube that carries air from the larynx to the lungs.
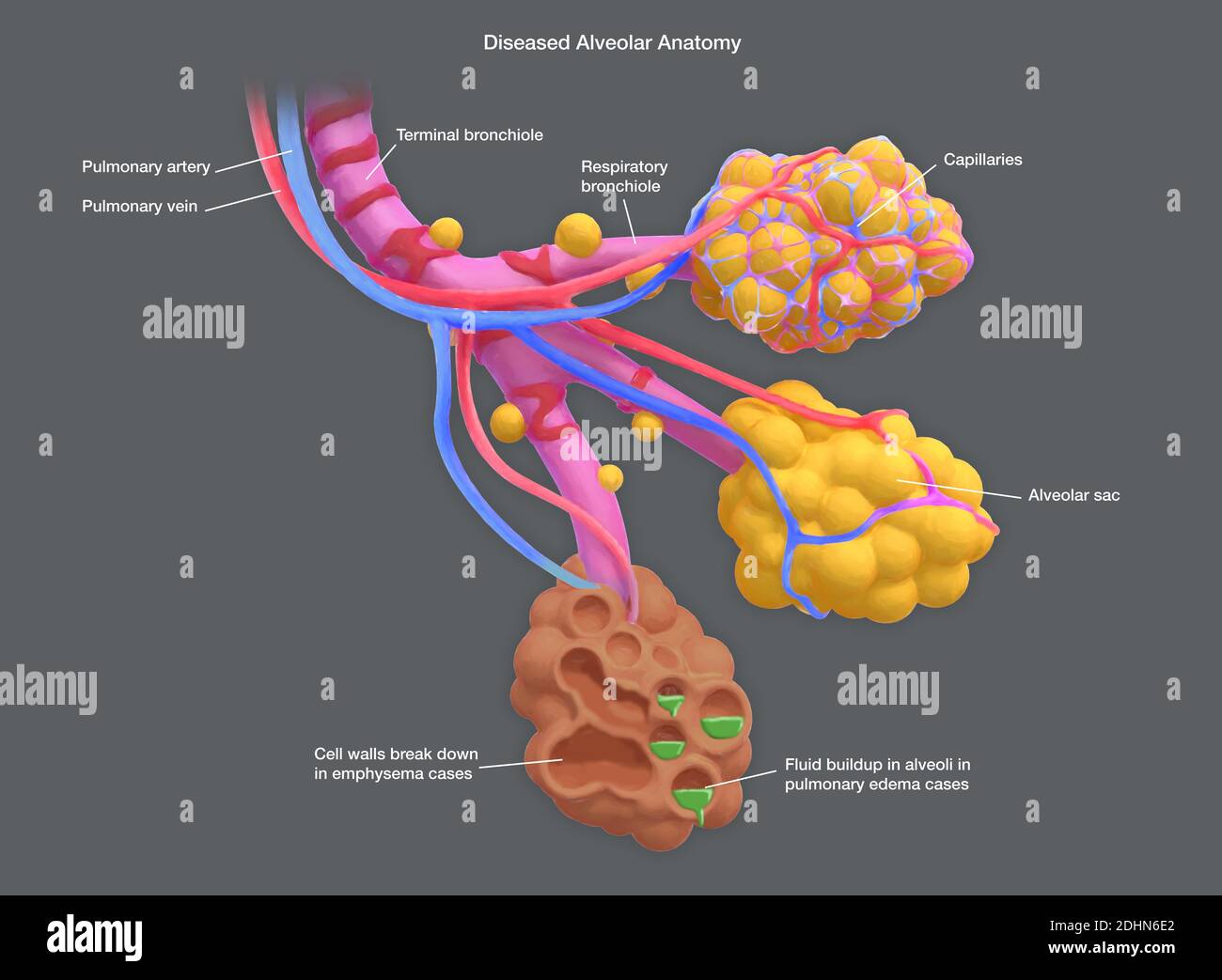
It branches into two main bronchi, one for each lung, which further divide into smaller bronchioles. The bronchioles terminate in tiny air sacs called alveoli, where gas exchange occurs.
The Role of Stroma and Alveolar Sacs in Gas Exchange, How does smoking affect your stroma and alveolar sacs
The stroma, a supporting framework of connective tissue, provides structure and support to the alveoli. The alveoli, tiny air sacs surrounded by capillaries, are the primary sites of gas exchange. Their thin walls and extensive surface area allow for efficient diffusion of oxygen from the inhaled air into the bloodstream and carbon dioxide from the blood into the alveoli to be exhaled.The process of gas exchange relies on the difference in partial pressure of oxygen and carbon dioxide between the alveoli and the blood.
Oxygen, with a higher partial pressure in the alveoli, diffuses across the alveolar-capillary membrane into the blood, while carbon dioxide, with a higher partial pressure in the blood, diffuses into the alveoli to be exhaled.
Smoking’s Impact on the Stroma
Smoking has a devastating impact on the delicate connective tissue of the lungs, known as the stroma. This intricate network of fibers and cells plays a crucial role in supporting the alveoli, the tiny air sacs where gas exchange occurs. Cigarette smoke disrupts the delicate balance of the stroma, leading to a cascade of harmful changes that compromise lung function.
Inflammation and Fibrosis in the Stroma
Cigarette smoke triggers an inflammatory response in the lungs, leading to the recruitment of immune cells like macrophages and neutrophils. These cells release inflammatory mediators, such as cytokines and chemokines, which contribute to the breakdown of the stroma. Chronic inflammation, a hallmark of smoking-related lung diseases, promotes the deposition of excess collagen, a protein that forms fibrous tissue. This process, known as fibrosis, stiffens the lung tissue, making it difficult for the lungs to expand and contract effectively.
Effects on Lung Elasticity and Expansion
The thickening and scarring of the stroma caused by fibrosis reduces the elasticity of the lungs, making it harder for them to inflate during inhalation. This leads to a decrease in lung volume and a reduction in the amount of oxygen that can be taken in. The thickened stroma also impedes the diffusion of oxygen and carbon dioxide across the alveolar walls, further compromising gas exchange.
As a result, smokers may experience shortness of breath, wheezing, and a persistent cough.
Smoking’s Effect on Alveolar Sacs
The alveolar sacs, tiny air pockets in the lungs, are where oxygen enters the bloodstream and carbon dioxide exits. Smoking significantly damages these crucial structures, hindering their ability to perform this vital gas exchange.
Alveolar Sac Damage
Smoking directly impacts the alveolar sacs, leading to various detrimental changes:
- Emphysema: This condition, characterized by the destruction of the walls of the alveoli, creates large, irregular air spaces. This results in a decrease in the surface area available for gas exchange, making it difficult for the lungs to absorb oxygen and expel carbon dioxide.
- Reduced Surface Area: Smoking triggers inflammation and irritation in the alveoli, leading to the production of excess mucus and the thickening of the alveolar walls. These changes further reduce the surface area available for gas exchange, making it harder for the body to get the oxygen it needs.
Impact on Gas Exchange Efficiency
The damage caused by smoking to the alveolar sacs directly impacts the efficiency of gas exchange.
- Reduced Oxygen Absorption: With a reduced surface area, the lungs struggle to absorb enough oxygen from the inhaled air. This leads to a chronic oxygen deficiency in the bloodstream, impacting various bodily functions.
- Impaired Carbon Dioxide Removal: The impaired gas exchange also hinders the removal of carbon dioxide from the blood. This can lead to a buildup of carbon dioxide in the body, leading to a condition called hypercapnia, which can be dangerous.
Respiratory Problems
The damage to the alveolar sacs caused by smoking can lead to various respiratory problems:
- Shortness of Breath: The reduced surface area for gas exchange and the difficulty in removing carbon dioxide can cause shortness of breath, even with minimal exertion.
- Chronic Obstructive Pulmonary Disease (COPD): Long-term smoking can lead to COPD, a progressive lung disease that makes it difficult to breathe.
- Wheezing and Coughing: Inflammation and irritation in the airways, caused by smoking, can lead to wheezing and coughing, particularly when exposed to irritants like smoke or dust.
The Role of Inflammation: How Does Smoking Affect Your Stroma And Alveolar Sacs
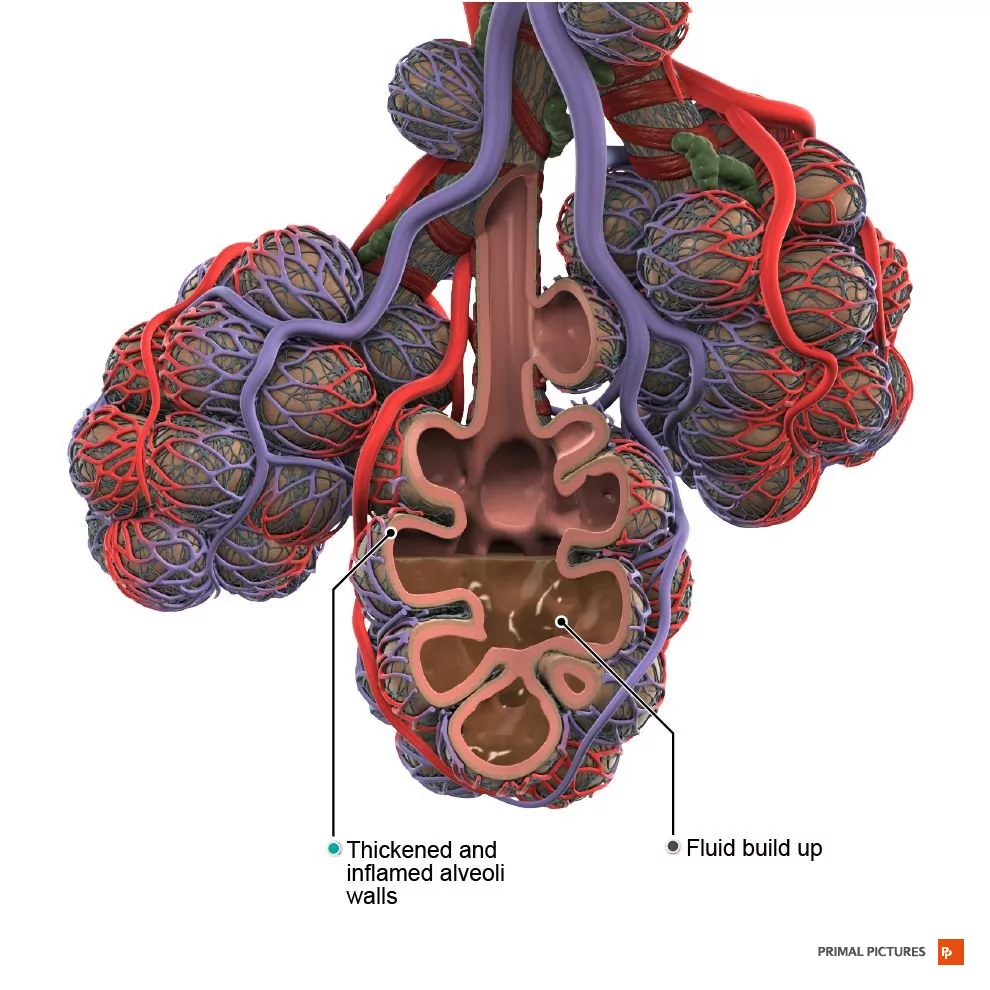
Cigarette smoke is a potent irritant, triggering an inflammatory response in the lungs. This response, while initially intended to protect the body, can become chronic and contribute significantly to the long-term damage of the stroma and alveolar sacs.The inflammatory response to cigarette smoke is complex and involves various immune cells. These cells are recruited to the lungs to fight off the harmful substances in smoke, but their prolonged presence can lead to tissue damage.
Inflammatory Cells Involved in Lung Damage
Chronic inflammation is a key factor in the development of chronic obstructive pulmonary disease (COPD), a serious lung condition characterized by airflow obstruction and lung damage.
- Neutrophils: These are the first responders to inflammation, releasing enzymes and reactive oxygen species that can damage lung tissue. They are often found in increased numbers in the airways of smokers.
- Macrophages: These cells engulf and digest foreign particles, including cigarette smoke components. However, prolonged exposure to smoke can lead to macrophage dysfunction, making them less effective at clearing debris and contributing to inflammation.
- T lymphocytes: These cells play a role in the immune response and can contribute to inflammation in the lungs. In smokers, T lymphocytes can become activated and release inflammatory cytokines, further exacerbating lung damage.
Smoking and Lung Cancer
Smoking is the leading cause of lung cancer, accounting for about 90% of cases. The link between smoking and lung cancer is undeniable, and the risk of developing the disease increases significantly with the amount and duration of smoking.
The Mechanism of Smoking-Induced Lung Cancer
The carcinogens in cigarette smoke damage DNA, leading to mutations that can cause uncontrolled cell growth and ultimately cancer.
- Direct DNA Damage: Carcinogens in smoke directly attack DNA, causing breaks and alterations in the genetic code. These mutations can disrupt the normal regulation of cell growth and division, leading to uncontrolled proliferation.
- Activation of Oncogenes: Some carcinogens can activate oncogenes, genes that promote cell growth and division. When these genes are abnormally activated, they can drive the development of cancer.
- Inactivation of Tumor Suppressor Genes: Carcinogens can also inactivate tumor suppressor genes, which normally act to prevent uncontrolled cell growth. Without these genes, cells can proliferate unchecked, leading to tumor formation.
Types of Lung Cancer Associated with Smoking
Smoking is linked to several types of lung cancer, including:
- Small Cell Lung Cancer (SCLC): This aggressive type of lung cancer is strongly associated with smoking and accounts for about 15% of all lung cancers. SCLC cells tend to grow rapidly and spread quickly to other parts of the body.
- Non-Small Cell Lung Cancer (NSCLC): This category encompasses a variety of lung cancers, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. NSCLC is also strongly associated with smoking and accounts for about 85% of all lung cancers.
Quitting Smoking

The decision to quit smoking is a powerful one, and your body will begin to heal and repair itself almost immediately. The benefits of quitting are numerous and far-reaching, impacting your overall health and well-being.
The Body’s Healing Journey
Within 20 minutes of quitting, your heart rate and blood pressure begin to drop, and circulation improves. Within 12 hours, the carbon monoxide levels in your blood decrease, and your oxygen levels increase. This means your body is already working to restore its natural balance.
Lung Repair and Improved Function
- Within a few weeks, your lungs begin to clear out mucus and debris, leading to improved breathing and reduced coughing.
- Over time, the cilia in your lungs, tiny hair-like structures that help clear out foreign particles, begin to function more effectively. This helps protect your lungs from future damage.
- Your lung capacity starts to increase, making it easier to breathe and engage in physical activities.
Reduced Risk of Cancer and Other Diseases
Quitting smoking significantly reduces your risk of developing various cancers, including lung, throat, bladder, and pancreatic cancer.
- The risk of heart disease, stroke, and other cardiovascular problems also decreases dramatically.
- Your risk of developing type 2 diabetes is reduced.
- Your overall risk of premature death is significantly lower compared to continuing to smoke.
The story of smoking’s impact on the stroma and alveolar sacs is a stark reminder of the delicate balance within our bodies. Understanding this intricate dance of damage and repair can empower us to make informed choices about our health. As we delve deeper into the consequences of smoking, we uncover a compelling narrative that underscores the importance of protecting our lungs, the silent heroes of our existence.
Query Resolution
What are the long-term effects of smoking on lung function?
Smoking can lead to chronic obstructive pulmonary disease (COPD), a progressive lung disease that makes it difficult to breathe. This can result in shortness of breath, wheezing, coughing, and other respiratory problems.
Can quitting smoking reverse lung damage?
While quitting smoking can’t completely undo the damage, your lungs can begin to heal and repair themselves. The benefits of quitting smoking are significant and can improve your overall health and quality of life.
Is there a specific type of lung cancer associated with smoking?
Smoking is a major risk factor for small cell lung cancer, a highly aggressive form of the disease. This type of cancer is often diagnosed at a later stage, making it more difficult to treat.






