How long for drugs to reach CD4+ cells stroma? This question lies at the heart of understanding drug efficacy in treating diseases that affect the immune system. The journey of a drug from administration to its target within the complex stromal microenvironment is a fascinating one, fraught with challenges and opportunities.
The stromal microenvironment, a rich tapestry of cells and extracellular matrix, plays a crucial role in immune regulation. CD4+ T cells, central players in immune responses, reside within this intricate network, making drug delivery to these cells a critical factor in treatment success. Understanding the factors that govern drug penetration into the stroma, including tissue barriers, cellular uptake mechanisms, and the influence of pharmacokinetic parameters, is essential for optimizing drug delivery and achieving therapeutic outcomes.
Drug Delivery to CD4+ Cells in the Stroma
Delivering drugs to CD4+ cells within the stromal microenvironment presents a significant challenge in treating diseases such as HIV infection. The stroma, a complex network of connective tissue and cells, provides a protective barrier for CD4+ cells, hindering the effective delivery of therapeutic agents. This section explores the different routes of drug administration, factors influencing drug penetration, and the challenges associated with targeting CD4+ cells within the stroma.
Routes of Drug Administration
The choice of drug administration route significantly influences the ability to reach CD4+ cells in the stroma.
- Oral Administration: Oral administration is a convenient and non-invasive route, but it often faces limitations in delivering drugs to the stroma due to first-pass metabolism and poor bioavailability. The gastrointestinal tract’s digestive enzymes and the liver’s metabolic processes can significantly reduce the drug concentration reaching the target site.
- Intravenous Administration: Intravenous administration bypasses the first-pass metabolism, achieving higher drug concentrations in the bloodstream. However, this route can be inconvenient and may require hospitalization. Additionally, the blood-brain barrier and other tissue barriers can hinder drug penetration into the stroma.
- Intramuscular Administration: Intramuscular injection provides a slower and more sustained release of drugs compared to intravenous administration. However, it may not be suitable for targeting specific stromal compartments.
- Subcutaneous Administration: Subcutaneous injection is a convenient and relatively painless route, but drug penetration into the stroma can be limited by the subcutaneous tissue’s barriers.
- Topical Administration: Topical administration is suitable for delivering drugs to the skin and mucous membranes but is not effective for targeting CD4+ cells in the stroma.
Factors Influencing Drug Penetration
Several factors influence the penetration of drugs into the stroma, impacting their effectiveness in reaching CD4+ cells.
- Tissue Barriers: The stroma is characterized by a dense extracellular matrix, consisting of collagen, elastin, and other proteins. These barriers can hinder drug diffusion and limit their access to CD4+ cells.
- Cellular Uptake Mechanisms: The ability of drugs to penetrate cell membranes and enter CD4+ cells depends on their physicochemical properties and the presence of specific transporters. Some drugs may require active transport mechanisms to cross cell membranes.
- Drug Properties: The size, charge, and lipophilicity of drugs significantly influence their ability to penetrate the stroma. Smaller, more lipophilic molecules tend to diffuse more readily through tissue barriers.
Challenges in Drug Delivery
Targeting CD4+ cells within the stromal microenvironment presents several challenges:
- Heterogeneity of the Stroma: The stroma is a complex and heterogeneous environment, with varying tissue composition and cellular density. This heterogeneity makes it difficult to achieve uniform drug distribution and target specific cell populations.
- Limited Drug Penetration: The dense extracellular matrix and cellular barriers can significantly hinder drug penetration into the stroma, reducing the drug concentration reaching CD4+ cells.
- Drug Resistance: CD4+ cells within the stroma can develop resistance to certain drugs, limiting their effectiveness in treating infections.
- Immune Response: Drug delivery systems can trigger an immune response, potentially leading to inflammation and tissue damage.
Pharmacokinetic Considerations
Understanding the pharmacokinetic profile of a drug is crucial for optimizing its delivery to CD4+ cells in the stroma. Pharmacokinetics encompasses the processes of absorption, distribution, metabolism, and elimination (ADME) that influence the drug’s concentration at the target site.
Drug Absorption
Drug absorption refers to the process by which a drug enters the bloodstream from its administration site. The route of administration, formulation, and physicochemical properties of the drug significantly influence its absorption. For example, oral administration often involves absorption from the gastrointestinal tract, while intravenous injection bypasses absorption altogether.
Drug Distribution
Once in the bloodstream, the drug distributes to various tissues and organs based on factors like blood flow, tissue permeability, and binding to plasma proteins. The stroma, being a relatively dense and complex tissue, presents challenges for drug distribution.
Drug Metabolism
Drug metabolism refers to the enzymatic transformation of the drug into metabolites. These metabolic processes, primarily occurring in the liver, can alter the drug’s activity, duration of action, and excretion.
Drug Elimination
Drug elimination encompasses the processes by which the drug and its metabolites are removed from the body. The primary routes of elimination are renal excretion (through the kidneys) and biliary excretion (through the bile).
Role of Drug Transporters and Efflux Pumps
Drug transporters and efflux pumps play critical roles in the movement of drugs across cell membranes, influencing drug distribution and accumulation within the stroma.
- Drug Transporters: These proteins facilitate the uptake of drugs into cells. For instance, the glucose transporter protein (GLUT1) facilitates the uptake of glucose into cells, and certain drug transporters can assist in the entry of drugs into CD4+ cells.
- Efflux Pumps: These proteins actively pump drugs out of cells, limiting drug accumulation and efficacy. For example, P-glycoprotein (P-gp), a prominent efflux pump, can transport a wide range of drugs out of cells, potentially hindering their entry into CD4+ cells.
Examples of Drugs Reaching CD4+ Cells in the Stroma
Several drugs have demonstrated efficacy in reaching CD4+ cells in the stroma. These drugs exhibit specific pharmacokinetic profiles that contribute to their ability to penetrate the stroma and target CD4+ cells.
- Antiretroviral Drugs: Antiretroviral drugs, used in the treatment of HIV infection, often target CD4+ cells. Some examples include:
- Tenofovir: This drug has good penetration into the stroma and can effectively reach CD4+ cells. It exhibits favorable pharmacokinetic properties, including a long half-life and good oral bioavailability.
- Efavirenz: This drug also demonstrates good penetration into the stroma and reaches CD4+ cells. It has a relatively long half-life and is primarily metabolized by the liver.
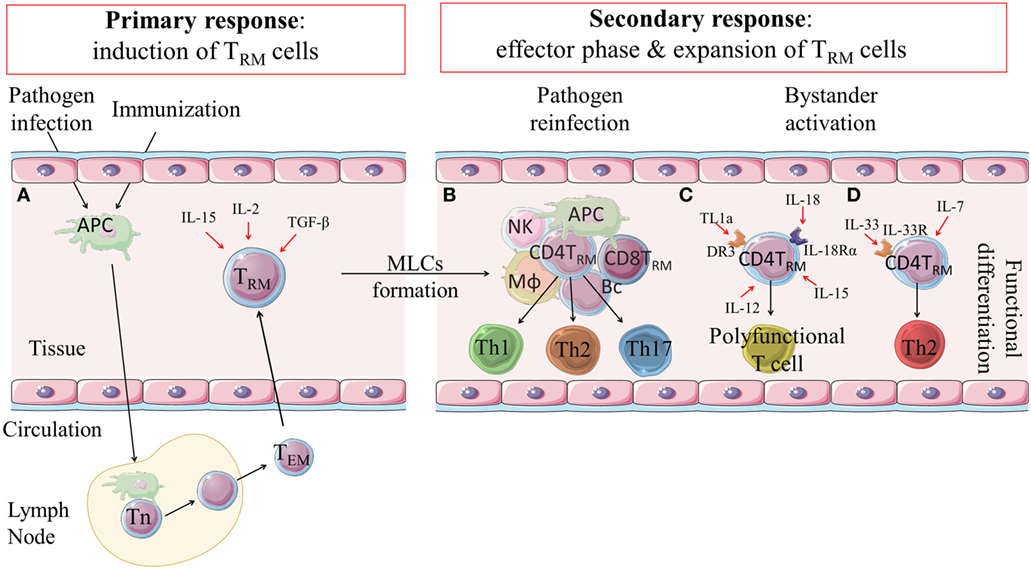
Cellular Interactions and Mechanisms: How Long For Drugs To Reach Cd4+ Cells Stroma
Understanding the cellular interactions and mechanisms by which drugs reach and interact with CD4+ cells in the stroma is crucial for optimizing drug delivery and therapeutic efficacy. This section delves into the specific receptors, signaling pathways, and drug-induced changes that govern drug action within this complex microenvironment.
Receptor-Mediated Drug Binding and Internalization
The initial step in drug action involves binding to specific receptors on the surface of CD4+ cells. This binding initiates a cascade of intracellular signaling events, ultimately leading to drug internalization and therapeutic effects.
- CCR5 and CXCR4 Receptors: These chemokine receptors are essential for HIV entry into CD4+ cells. Drugs targeting these receptors, such as maraviroc and enfuvirtide, block viral entry and prevent infection.
- Transferrin Receptor: This receptor mediates the uptake of iron-containing proteins, including transferrin. Drugs conjugated to transferrin can exploit this pathway to enhance delivery to CD4+ cells, particularly in the context of iron deficiency.
- Fc Receptors: These receptors bind to antibodies and play a role in immune responses. Drugs conjugated to antibodies can utilize Fc receptors to target CD4+ cells and enhance their therapeutic efficacy.
Drug-Induced Signaling Pathways
Upon binding to their respective receptors, drugs trigger intracellular signaling cascades that modulate various cellular processes. These pathways can influence gene expression, cell survival, and immune responses.
- MAPK Pathway: This pathway is involved in cell growth, differentiation, and survival. Certain drugs activate MAPK signaling, promoting CD4+ cell proliferation and survival.
- PI3K/Akt Pathway: This pathway regulates cell survival, growth, and metabolism. Drugs targeting this pathway can enhance CD4+ cell survival and inhibit apoptosis.
- NF-κB Pathway: This pathway plays a crucial role in inflammation and immune responses.
Drugs that modulate NF-κB signaling can influence CD4+ cell activation and cytokine production.
Drug-Induced Changes in the Stromal Microenvironment
Drugs can also alter the stromal microenvironment, potentially influencing CD4+ cell function and therapeutic outcomes.
- Immune Cell Recruitment: Some drugs may attract immune cells to the stroma, enhancing inflammation and potentially aiding in the clearance of pathogens.
- Matrix Remodeling: Drugs can influence the composition and structure of the extracellular matrix, affecting cell migration and adhesion.
- Cytokine Production: Drugs can modulate cytokine production by stromal cells, impacting the overall immune response and potentially influencing CD4+ cell function.
Imaging Techniques for Monitoring Drug Delivery

Visualizing and tracking the delivery of drugs to CD4+ cells in the stroma is crucial for understanding drug distribution, efficacy, and potential off-target effects. Various imaging techniques have been employed to address this challenge, providing valuable insights into the pharmacokinetic and pharmacodynamic aspects of drug delivery in the stromal microenvironment.
Overview of Imaging Techniques
Imaging techniques play a vital role in understanding drug delivery to CD4+ cells within the stromal microenvironment. These techniques offer the ability to visualize and track drug distribution, localization, and interactions with target cells, providing valuable insights into drug efficacy and potential off-target effects.
- Fluorescence Microscopy: This technique utilizes fluorescent probes, often conjugated to drugs, to visualize the drug’s distribution and localization within the stroma. The fluorescence signal emitted by the probe can be detected using a fluorescence microscope, allowing for real-time imaging of drug delivery. Fluorescence microscopy is particularly useful for studying the uptake and trafficking of drugs within cells and tissues.
- Confocal Microscopy: Confocal microscopy offers enhanced spatial resolution compared to traditional fluorescence microscopy.
It uses a laser beam to illuminate a specific focal plane, eliminating out-of-focus light and providing high-quality images of the stromal microenvironment. Confocal microscopy is valuable for studying the distribution of drugs in three dimensions, particularly in complex tissues like lymph nodes.
- Two-Photon Microscopy: This technique uses two photons of lower energy to excite fluorescent probes, allowing for deeper tissue penetration than traditional confocal microscopy.
Two-photon microscopy is particularly useful for studying drug delivery in thick tissues, such as lymph nodes and tumors.
- Magnetic Resonance Imaging (MRI): MRI utilizes magnetic fields and radio waves to create detailed images of the body. MRI can be used to visualize the distribution of drugs in the stroma, particularly those that are labeled with paramagnetic contrast agents. MRI is particularly valuable for studying drug delivery in large animal models and human subjects.
- Positron Emission Tomography (PET): PET involves the administration of radioactive tracers, often conjugated to drugs, and detects the emitted positrons to create images of drug distribution. PET is particularly sensitive for visualizing drug accumulation in specific tissues and organs.
Examples of Imaging Studies
Numerous imaging studies have provided valuable insights into drug delivery to CD4+ cells in the stroma.
- Fluorescence Microscopy Studies: Researchers have used fluorescence microscopy to track the delivery of fluorescently labeled antiretroviral drugs to CD4+ cells in lymph nodes. These studies have revealed that antiretroviral drugs can accumulate in the lymph node stroma and penetrate into the T cell zones, where CD4+ cells reside.
- Confocal Microscopy Studies: Confocal microscopy has been employed to study the distribution of antiretroviral drugs in lymph nodes.
These studies have demonstrated that antiretroviral drugs can be found in the lymph node stroma, as well as within CD4+ cells.
- Two-Photon Microscopy Studies: Two-photon microscopy has been used to visualize the delivery of fluorescently labeled antiretroviral drugs to CD4+ cells in the lymph nodes of living animals. These studies have provided insights into the dynamics of drug delivery and the interaction of drugs with CD4+ cells in the stromal microenvironment.
- MRI Studies: MRI studies have been conducted to assess the distribution of antiretroviral drugs in the lymph nodes of human subjects. These studies have shown that antiretroviral drugs can accumulate in the lymph node stroma and penetrate into the T cell zones.
- PET Studies: PET studies have been used to track the delivery of radioactive tracers conjugated to antiretroviral drugs to CD4+ cells in the lymph nodes of human subjects.
These studies have provided insights into the pharmacokinetics of drug delivery and the distribution of drugs in the stromal microenvironment.
Advantages and Limitations of Imaging Approaches
Each imaging technique offers distinct advantages and limitations for monitoring drug delivery to CD4+ cells in the stroma.
| Technique | Advantages | Limitations |
|---|---|---|
| Fluorescence Microscopy | High sensitivity, relatively inexpensive, can be used in live cells and tissues | Limited tissue penetration, can be affected by autofluorescence |
| Confocal Microscopy | Enhanced spatial resolution, can visualize drug distribution in three dimensions | Limited tissue penetration, can be expensive |
| Two-Photon Microscopy | Deep tissue penetration, can be used in live cells and tissues | Can be expensive, requires specialized equipment |
| MRI | Non-invasive, can be used in large animal models and human subjects | Limited sensitivity, can be affected by motion artifacts |
| PET | High sensitivity, can visualize drug accumulation in specific tissues and organs | Requires radioactive tracers, can be expensive |
Therapeutic Applications and Future Directions
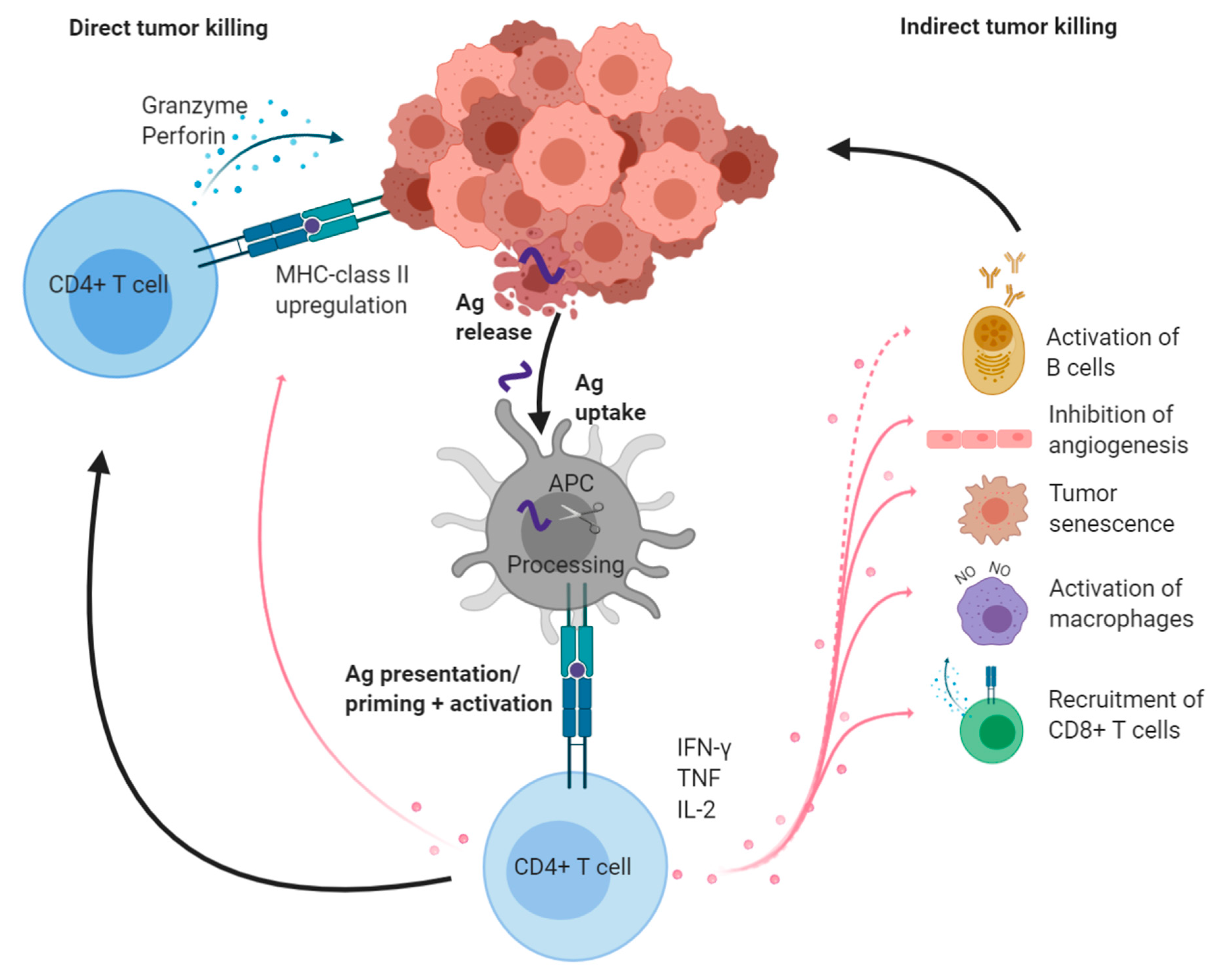
Targeting CD4+ cells in the stroma holds significant promise for treating a range of diseases, particularly those involving immune dysregulation. The ability to deliver drugs directly to these cells offers a unique opportunity to modulate immune responses at the site of inflammation, potentially leading to more targeted and effective therapies.
Therapeutic Applications
The therapeutic potential of drugs targeting CD4+ cells in the stroma extends to various disease areas.
- Infectious Diseases: Targeting CD4+ cells in the stroma could enhance the efficacy of antiretroviral therapy (ART) in HIV-infected individuals. By delivering antiretroviral drugs directly to the site of HIV replication in lymphoid tissues, this approach could potentially suppress viral load more effectively and reduce the risk of viral reservoirs.
- Autoimmune Disorders: Targeting CD4+ cells in the stroma could be a promising strategy for treating autoimmune disorders like rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel disease. By delivering immunosuppressive drugs directly to the inflamed tissues, this approach could help to suppress the autoimmune response and reduce inflammation.
- Cancer Immunotherapy: Targeting CD4+ cells in the stroma could enhance the effectiveness of cancer immunotherapy by promoting the recruitment and activation of cytotoxic T lymphocytes (CTLs) to the tumor microenvironment. This approach could help to overcome the immunosuppressive environment often found in tumors and enhance the antitumor immune response.
Challenges and Opportunities
While the potential of targeting CD4+ cells in the stroma is significant, several challenges need to be addressed.
- Delivery Barriers: The stroma is a dense and complex environment, making it challenging to deliver drugs effectively to CD4+ cells. The extracellular matrix (ECM) can hinder drug diffusion, and the tight junctions between cells can prevent drug entry.
- Drug Stability: Drugs delivered to the stroma may be susceptible to degradation by enzymes or other factors present in the microenvironment. This can reduce the effectiveness of the treatment.
- Off-target Effects: Delivering drugs to CD4+ cells in the stroma may result in off-target effects, potentially leading to unintended consequences.
Novel Drug Delivery Strategies, How long for drugs to reach cd4+ cells stroma
To overcome these challenges, researchers are exploring novel drug delivery strategies that can enhance the effectiveness of drug targeting to CD4+ cells in the stroma.
- Nanoparticle-Based Delivery: Nanoparticles can be designed to encapsulate drugs and target them specifically to CD4+ cells in the stroma. This approach can improve drug stability, enhance drug penetration through the ECM, and reduce off-target effects.
- Antibody-Conjugated Delivery: Antibodies that specifically bind to CD4+ cells can be used to deliver drugs directly to these cells. This approach can improve drug targeting and enhance the therapeutic effect.
- Gene Therapy: Gene therapy can be used to modify CD4+ cells in the stroma to express therapeutic proteins or to silence genes involved in disease pathogenesis. This approach offers a long-term solution for treating diseases by targeting the underlying cause.
Key Characteristics of Drugs Targeting CD4+ Cells in the Stroma
| Characteristic | Description |
|---|---|
| Mechanism of Action | Modulate immune responses by targeting CD4+ cells in the stroma, affecting cytokine production, T cell activation, and immune cell trafficking. |
| Therapeutic Applications | Infectious diseases, autoimmune disorders, cancer immunotherapy. |
| Limitations | Delivery barriers, drug stability, off-target effects. |
Navigating the intricacies of drug delivery to CD4+ cells in the stroma is a complex undertaking, but one that holds immense promise for improving patient outcomes. By unraveling the mechanisms of drug transport, cellular interactions, and the dynamic interplay within the stromal microenvironment, we can unlock the potential of targeted therapies. As we continue to refine our understanding of these processes, we can pave the way for more effective and personalized treatment strategies.
Helpful Answers
What are the common routes of drug administration for targeting CD4+ cells in the stroma?
Common routes include oral, intravenous, subcutaneous, and topical administration, each with its own advantages and disadvantages in terms of drug penetration and bioavailability.
What are some examples of drugs known to effectively reach CD4+ cells in the stroma?
Examples include antiretroviral drugs for HIV infection, immunosuppressants for autoimmune diseases, and certain cancer therapies.
How do imaging techniques help in monitoring drug delivery to CD4+ cells?
Imaging techniques like PET scans, MRI, and fluorescence microscopy allow visualization of drug distribution and localization within the stromal microenvironment, providing valuable insights into drug uptake and efficacy.






