Is stroma only connective tissue? Well, that’s like asking if a dog is just a furry friend – it’s partially true, but there’s so much more to the story! Stroma, the supporting structure of organs, is indeed built on a foundation of connective tissue, but it’s a bustling city with a cast of characters and a complex web of interactions.
Think of it like the scaffolding holding up a magnificent building – it might not be the flashiest part, but it’s essential for the whole structure to stand tall.
We’ll dive into the fascinating world of stroma, exploring its diverse inhabitants, from the hardworking fibroblasts to the stealthy macrophages, and uncover the secrets of the extracellular matrix, a gooey, fibrous substance that holds it all together. Get ready to learn how stroma, despite being often overlooked, plays a crucial role in keeping organs functioning smoothly and even impacts how diseases develop.
Buckle up, it’s going to be a wild ride!
Components of Stroma
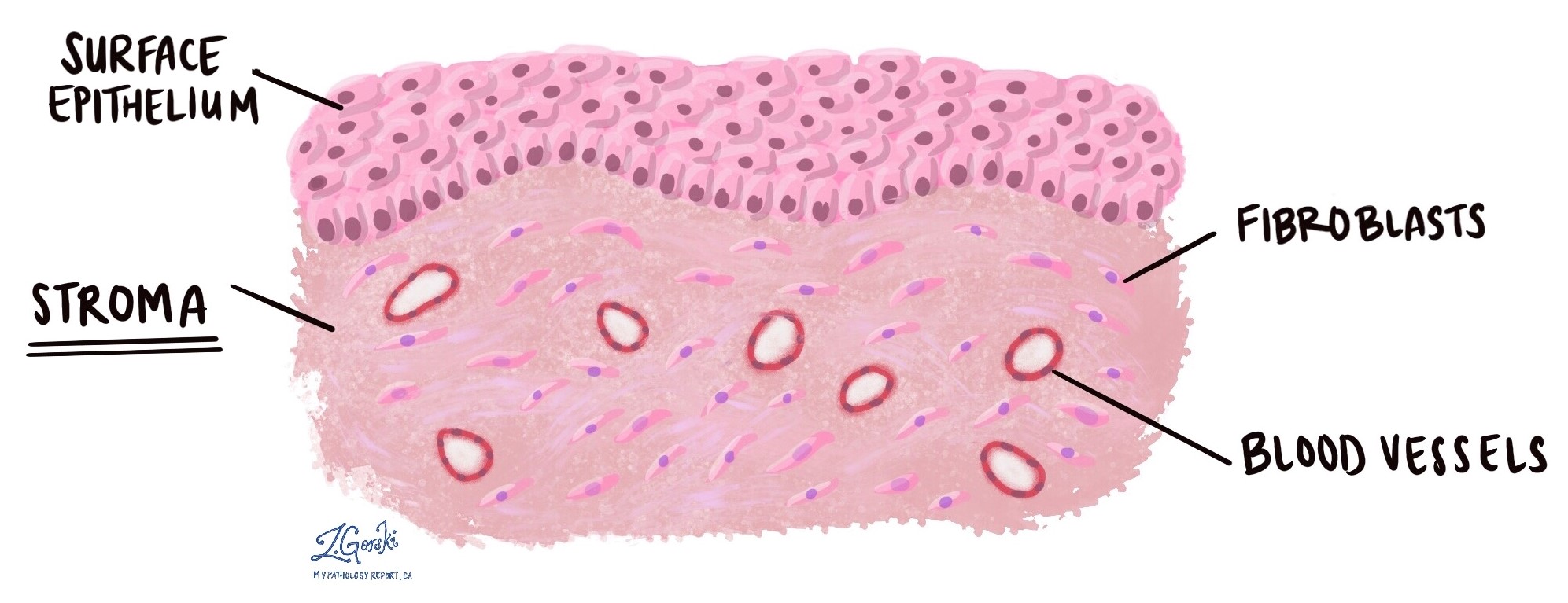
Stroma, the supporting framework of organs and tissues, is composed of connective tissue that provides structural integrity and facilitates communication between cells. This intricate network of cells and extracellular matrix plays a vital role in maintaining tissue function and homeostasis.
Cellular Components of Stroma
The cellular components of stroma are responsible for synthesizing, maintaining, and modifying the extracellular matrix. They contribute to the diverse functions of the stroma, from providing structural support to facilitating immune responses.
- Fibroblasts are the primary cells responsible for synthesizing and secreting the components of the extracellular matrix, including collagen, elastin, and proteoglycans. They are spindle-shaped cells with elongated nuclei and abundant rough endoplasmic reticulum, reflecting their active role in protein synthesis. Fibroblasts are crucial for maintaining the structural integrity of tissues and facilitating tissue repair.
- Macrophages are phagocytic cells that engulf and digest cellular debris, pathogens, and foreign substances. They play a crucial role in immune defense and tissue remodeling. Macrophages are derived from monocytes and reside in the stroma, where they continuously monitor the surrounding environment for potential threats.
- Mast cells are immune cells that release histamine and other inflammatory mediators in response to allergens or pathogens. They are characterized by their large, granulated cytoplasm and are involved in allergic reactions and defense against parasites.
- Adipocytes are specialized cells that store lipids, providing energy reserves and insulation. They are found in various tissues, including the stroma of adipose tissue and certain organs.
- Pericytes are multipotent cells that surround blood vessels and contribute to vascular stability and angiogenesis. They can differentiate into various cell types, including fibroblasts, smooth muscle cells, and endothelial cells.
Extracellular Matrix Composition
The extracellular matrix is a complex network of proteins and polysaccharides that provides structural support, regulates cell behavior, and facilitates communication between cells. It is composed of two main components: fibers and ground substance.
Fibers
Fibers provide tensile strength, elasticity, and structural support to the stroma. They are composed of proteins that assemble into long, filamentous structures.
- Collagen fibers are the most abundant type of fiber in the extracellular matrix. They are strong and flexible, providing tensile strength and resistance to stretching. There are numerous types of collagen fibers, each with specific properties and functions.
- Elastin fibers are highly elastic, allowing tissues to stretch and recoil. They are found in tissues that require flexibility, such as skin, blood vessels, and lungs.
- Reticular fibers are thin, branching fibers composed of type III collagen. They form delicate networks that support cells and tissues, particularly in lymphoid organs and the liver.
Ground Substance
Ground substance is a gel-like material that fills the spaces between cells and fibers. It provides a medium for cell migration, nutrient exchange, and signaling.
- Proteoglycans are large molecules composed of protein core chains attached to glycosaminoglycans (GAGs). GAGs are long, unbranched polysaccharide chains that attract water, contributing to the gel-like consistency of ground substance. Proteoglycans play a role in regulating water content, cell adhesion, and signaling.
- Glycosaminoglycans (GAGs) are negatively charged polysaccharides that attract water and cations, creating a hydrated environment that facilitates diffusion and cell migration. They are also involved in regulating cell adhesion and signaling.
- Adhesive glycoproteins, such as fibronectin and laminin, mediate cell-cell and cell-matrix interactions. They bind to cell surface receptors and to components of the extracellular matrix, promoting cell adhesion, migration, and signaling.
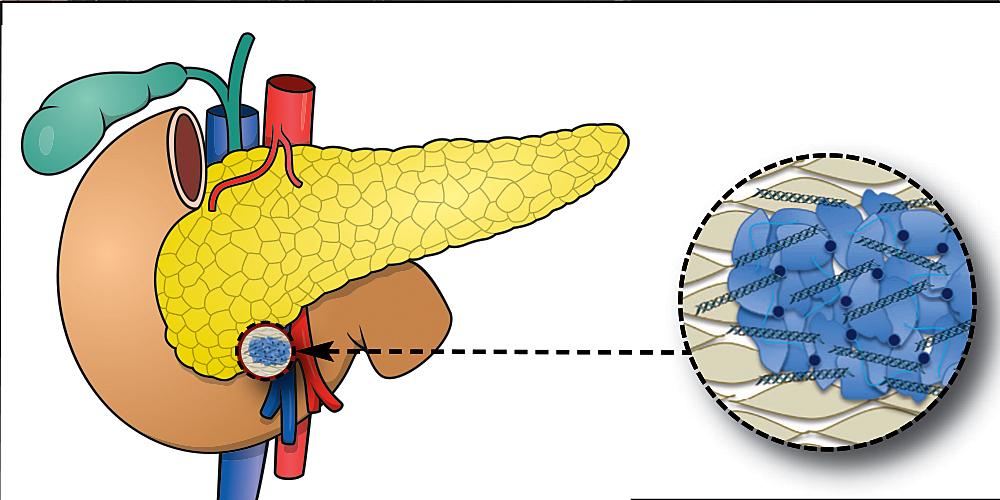
Stroma in Specific Organs

The stroma, the supporting framework of an organ, plays a crucial role in providing structural integrity, facilitating communication between cells, and regulating tissue function. It varies in composition and organization depending on the specific organ’s needs.
Stroma in Specific Organs
The composition of the stroma varies depending on the specific organ and its function. Here is a table showcasing examples of different organs and their respective stroma components:
| Organ | Cell Types | Extracellular Matrix | Function |
|---|---|---|---|
| Liver | Hepatic stellate cells, Kupffer cells, fibroblasts | Collagen, elastin, hyaluronic acid | Provides structural support, regulates blood flow, and detoxifies the blood. |
| Kidney | Mesangial cells, pericytes, fibroblasts | Collagen, laminin, fibronectin | Supports the glomerulus, filters blood, and regulates blood flow. |
| Lung | Fibroblasts, smooth muscle cells, mast cells | Collagen, elastin, proteoglycans | Provides structural support, maintains airway patency, and facilitates gas exchange. |
| Heart | Cardiac fibroblasts, endothelial cells, smooth muscle cells | Collagen, elastin, glycosaminoglycans | Provides structural support, regulates blood flow, and facilitates electrical conduction. |
| Brain | Astrocytes, microglia, oligodendrocytes | Collagen, laminin, hyaluronic acid | Supports neurons, regulates blood flow, and protects the brain from injury. |
Stroma and Disease: Is Stroma Only Connective Tissue
The stroma, while often overlooked, plays a crucial role in maintaining tissue homeostasis and influencing disease progression. Changes in stromal architecture and function can significantly contribute to the development and progression of various diseases, making the stroma a potential target for therapeutic intervention.
Stromal Alterations in Disease
The stroma is not a passive bystander in disease processes. Its composition and function can be dramatically altered in response to disease states, often contributing to the pathogenesis. These alterations can manifest in various ways, including:
- Increased Stromal Cell Density: In many diseases, the stroma becomes denser, with an increase in the number of stromal cells, such as fibroblasts and myofibroblasts. This increased density can contribute to tissue stiffness and impede the diffusion of nutrients and oxygen, further exacerbating the disease process. For instance, in fibrosis, the excessive accumulation of fibroblasts and extracellular matrix components leads to tissue scarring and dysfunction.
- Altered Extracellular Matrix Composition: The extracellular matrix (ECM) is a critical component of the stroma, providing structural support and regulating cell behavior. In disease, the ECM composition can be altered, leading to changes in tissue stiffness, cell adhesion, and signaling pathways. For example, in cancer, the ECM can be remodeled by tumor cells to promote invasion and metastasis.
- Inflammation and Immune Cell Infiltration: The stroma can be infiltrated by immune cells, such as macrophages and lymphocytes, in response to disease. These immune cells can contribute to tissue damage and inflammation, further promoting disease progression. For example, in rheumatoid arthritis, the synovium, a specialized stromal tissue, is infiltrated by immune cells, leading to joint inflammation and destruction.
- Altered Vascularization: The stroma provides the vascular network that supplies tissues with nutrients and oxygen. In disease, the vascularization of the stroma can be altered, leading to hypoxia and impaired tissue function. For example, in tumor growth, the tumor microenvironment often exhibits abnormal vascularization, promoting tumor growth and metastasis.
Examples of Diseases with Stromal Alterations
Numerous diseases are characterized by significant stromal alterations, highlighting the critical role of the stroma in disease pathogenesis.
- Cancer: The tumor microenvironment, which includes the stroma, plays a crucial role in tumor growth, invasion, and metastasis. Stromal cells can be reprogrammed by tumor cells to promote angiogenesis, immune suppression, and ECM remodeling, all contributing to tumor progression. For instance, in breast cancer, the stroma can be infiltrated by myofibroblasts, which promote tumor growth and invasion.
- Fibrosis: Fibrosis is a pathological process characterized by excessive deposition of ECM components, leading to tissue scarring and dysfunction. This process often involves significant stromal alterations, with increased fibroblast activity and altered ECM composition. Examples include liver fibrosis, lung fibrosis, and kidney fibrosis.
- Arthritis: In rheumatoid arthritis, the synovium, a specialized stromal tissue, undergoes significant alterations, including inflammation, immune cell infiltration, and ECM remodeling. These changes contribute to joint inflammation, cartilage destruction, and bone erosion.
- Neurodegenerative Diseases: The stroma in the central nervous system, known as the glial cells, can be altered in neurodegenerative diseases. These alterations can contribute to neuronal dysfunction and death. For example, in Alzheimer’s disease, astrocytes, a type of glial cell, can become reactive and contribute to the formation of amyloid plaques, a hallmark of the disease.
Therapeutic Targets in Stroma, Is stroma only connective tissue
The understanding of the role of the stroma in disease has opened up new avenues for therapeutic intervention. Targeting stromal alterations offers a promising approach for treating various diseases, including:
- Anti-fibrotic Therapies: Targeting the excessive deposition of ECM components and fibroblast activation is a promising strategy for treating fibrosis. Several anti-fibrotic drugs are under development, targeting various signaling pathways involved in fibroblast activation and ECM production.
- Cancer Therapies: Targeting the tumor microenvironment, including the stroma, is emerging as a critical strategy for cancer treatment. Strategies include inhibiting angiogenesis, targeting stromal cell signaling pathways, and promoting immune cell infiltration to the tumor microenvironment.
- Immunomodulatory Therapies: Targeting the immune response in the stroma can be beneficial in diseases with an inflammatory component. For example, in rheumatoid arthritis, therapies targeting the inflammatory cytokines and immune cell infiltration in the synovium can reduce inflammation and joint damage.
So, the next time you think of an organ, remember it’s not just the fancy cells doing all the work. There’s a whole hidden world of connective tissue, a bustling metropolis of stroma, supporting and shaping the entire operation. It’s like the unsung heroes of the body, quietly making sure everything runs smoothly. And who knows, maybe one day, we’ll even learn to harness the power of stroma to fight disease and keep our bodies healthy for years to come.
Now that’s something worth celebrating!
General Inquiries
Is stroma always visible under a microscope?
Not necessarily! Sometimes, it’s pretty transparent, but you can often see the fibers and cells that make up stroma with special staining techniques.
What’s the difference between stroma and parenchyma?
Think of parenchyma as the “functional” part of an organ – the cells that do the main job, like producing hormones or filtering blood. Stroma is the “support system” – the connective tissue that holds the parenchyma together and provides structural support.
Can stroma be affected by aging?
Absolutely! Stroma can become less flexible and less efficient as we age, which can contribute to age-related changes in organs.






