What does echogenic stroma mean? It’s a question that often pops up when you’re looking at ultrasound images, especially during pregnancy. In a nutshell, echogenic stroma refers to areas that appear brighter than usual on an ultrasound. These areas can be caused by a variety of things, from normal tissues to abnormal growths. Understanding the meaning of echogenic stroma can help doctors make informed decisions about your health.
This article dives into the world of echogenic stroma, explaining its significance in different medical contexts, exploring its causes, and examining how it appears in various organs. We’ll also discuss the role of echogenic stroma in pregnancy and what it means for your health. So buckle up, and let’s explore the fascinating world of echogenic stroma together!
Echogenic Stroma
Echogenic stroma refers to a bright, white area observed on ultrasound imaging. It is characterized by a high level of sound wave reflection, which creates a bright signal on the ultrasound screen. This bright appearance is often associated with increased density or a higher concentration of collagen fibers in the tissue.
Significance of Echogenic Stroma
The significance of echogenic stroma varies depending on the specific organ or tissue being examined. In some cases, it may be a normal finding, while in others, it can be indicative of underlying pathology.
- In the context of the uterus, echogenic stroma can be a normal finding, particularly in the endometrial lining during the menstrual cycle. However, in some cases, it may also indicate conditions such as fibroids, adenomyosis, or endometrial polyps.
- In the breast, echogenic stroma can be a normal finding in the dense breast tissue. However, it may also be associated with fibroadenomas, cysts, or malignancies.
- In the prostate, echogenic stroma is often seen in benign prostatic hyperplasia (BPH). However, it may also be associated with prostate cancer.
- In the thyroid, echogenic stroma is commonly observed in nodules. The presence of echogenic stroma can help differentiate between benign and malignant nodules.
Examples of Medical Conditions
Here are some specific examples of medical conditions where echogenic stroma is observed:
- Fibroids: These are noncancerous growths in the uterus that can be associated with echogenic stroma. Fibroids are often seen as well-defined, round or oval masses with a heterogeneous echogenic pattern.
- Adenomyosis: This condition occurs when the endometrial tissue grows into the uterine muscle wall. It can cause pain, heavy bleeding, and may appear as echogenic stroma within the uterine myometrium.
- Endometrial polyps: These are growths in the lining of the uterus that can be associated with echogenic stroma. Polyps can be seen as a well-defined, echogenic mass protruding into the uterine cavity.
- Breast fibroadenomas: These are noncancerous tumors in the breast that can be associated with echogenic stroma. Fibroadenomas are often seen as well-defined, round or oval masses with a heterogeneous echogenic pattern.
- Prostate cancer: This type of cancer can be associated with echogenic stroma, particularly in the peripheral zone of the prostate. However, it’s important to note that not all echogenic areas in the prostate are cancerous.
- Thyroid nodules: Echogenic stroma can be present in both benign and malignant thyroid nodules. The presence of echogenic stroma alone is not diagnostic of cancer, but it can be a helpful clue for further investigation.
Echogenic Stroma in Ultrasound Imaging

Echogenic stroma, characterized by increased echogenicity, is a common finding in ultrasound imaging. It represents a dense, fibrous tissue that reflects sound waves more effectively than surrounding tissues, resulting in a brighter appearance on the ultrasound image.
Echogenicity Levels in Ultrasound
The appearance of echogenic stroma on ultrasound images is determined by its echogenicity level, which refers to the brightness of the tissue on the image. Echogenicity levels are categorized as follows:
- Hypoechoic: Tissues that appear darker than surrounding tissues. These tissues reflect sound waves less effectively, resulting in a lower signal intensity on the ultrasound image.
- Hyperechoic: Tissues that appear brighter than surrounding tissues. These tissues reflect sound waves more effectively, resulting in a higher signal intensity on the ultrasound image.
- Isoechoic: Tissues that have the same echogenicity as surrounding tissues. These tissues reflect sound waves similarly to surrounding tissues, resulting in a similar signal intensity on the ultrasound image.
Echogenic stroma is typically hyperechoic, appearing brighter than the surrounding tissues. However, the degree of echogenicity can vary depending on the specific tissue and the ultrasound machine settings.
The Role of Ultrasound in Identifying and Characterizing Echogenic Stroma
Ultrasound plays a crucial role in identifying and characterizing echogenic stroma. It allows for real-time visualization of the tissue and provides information about its size, shape, and location. Ultrasound can also help differentiate echogenic stroma from other tissues with similar appearances, such as tumors or cysts.Ultrasound can be used to:
- Identify the presence of echogenic stroma: By observing the hyperechoic appearance of the tissue, ultrasound can detect the presence of echogenic stroma.
- Determine the size and shape of echogenic stroma: Ultrasound images provide information about the dimensions and contours of the tissue, helping to assess its size and shape.
- Evaluate the location of echogenic stroma: Ultrasound images can pinpoint the exact location of the echogenic stroma within the body, aiding in the diagnosis and treatment planning.
- Differentiate echogenic stroma from other tissues: Ultrasound can help distinguish echogenic stroma from other tissues with similar appearances, such as tumors or cysts.
Ultrasound is a valuable tool for assessing echogenic stroma, providing essential information for diagnosis and treatment planning.
Causes of Echogenic Stroma
Echogenic stroma, characterized by increased brightness on ultrasound imaging, can arise from various factors affecting the tissue’s composition and structure. Understanding the underlying causes is crucial for accurate diagnosis and management of associated conditions.
Common Causes of Echogenic Stroma in Various Organs
Echogenic stroma can occur in different organs, each with its own set of potential causes. Here are some common examples:
- Ovaries: Increased echogenicity in ovarian stroma can be associated with various conditions, including polycystic ovary syndrome (PCOS), fibroids, and ovarian cysts. In PCOS, the stroma may become thickened and echogenic due to hormonal imbalances and increased androgen production. Fibroids, benign tumors of the uterus, can also cause echogenic stroma in the ovaries. Ovarian cysts, fluid-filled sacs within the ovary, can sometimes have echogenic walls due to inflammation or other factors.
- Uterus: Echogenic stroma in the uterine wall can be a sign of fibroids, endometriosis, or other conditions. Fibroids, as mentioned earlier, can cause increased echogenicity in the uterine stroma. Endometriosis, a condition where endometrial tissue grows outside the uterus, can also lead to echogenic stroma in the uterine wall. Other causes include inflammation, infections, and scarring.
- Prostate: In the prostate, echogenic stroma can be a sign of benign prostatic hyperplasia (BPH), prostatitis, or prostate cancer. BPH, an enlargement of the prostate gland, can cause increased echogenicity due to tissue proliferation. Prostatitis, inflammation of the prostate, can also lead to echogenic stroma. Prostate cancer, a malignant tumor of the prostate, can also manifest as echogenic stroma on ultrasound imaging.
- Breast: Echogenic stroma in the breast can be associated with various conditions, including fibrocystic changes, fibroadenomas, and breast cancer. Fibrocystic changes, a common condition characterized by cysts and fibrous tissue in the breast, can cause increased echogenicity in the breast stroma. Fibroadenomas, benign tumors of the breast, can also appear echogenic on ultrasound. Breast cancer, a malignant tumor of the breast, can also present with echogenic stroma, but further investigations are required for definitive diagnosis.
Underlying Pathophysiological Mechanisms
Echogenic stroma formation is often related to changes in tissue composition and structure. These changes can include:
- Increased tissue density: Fibrosis, a process involving the formation of excessive fibrous connective tissue, can lead to increased tissue density and echogenicity. This can occur due to inflammation, injury, or chronic disease processes.
- Cellular proliferation: Increased cell numbers, as seen in conditions like fibroids or BPH, can also contribute to echogenic stroma. The denser cell population reflects more ultrasound waves, resulting in increased brightness.
- Deposition of calcium: Calcifications, often associated with aging or certain diseases, can significantly increase tissue echogenicity. These deposits reflect ultrasound waves more strongly, creating a bright appearance on the image.
- Vascular changes: Altered blood flow patterns, such as decreased perfusion or increased vascularity, can also influence echogenicity. These changes can be associated with inflammation, tumor growth, or other conditions.
Examples of Diseases and Conditions Associated with Echogenic Stroma
Echogenic stroma can be a feature of various diseases and conditions, including:
- Polycystic ovary syndrome (PCOS): Characterized by multiple cysts in the ovaries, PCOS can cause echogenic stroma due to hormonal imbalances and increased androgen production. The stroma may appear thickened and echogenic on ultrasound.
- Fibroids: Benign tumors of the uterus, fibroids can cause echogenic stroma due to their fibrous nature. They can be found in the uterine wall, the submucosal layer, or the serosal layer.
- Endometriosis: A condition where endometrial tissue grows outside the uterus, endometriosis can cause echogenic stroma in the uterine wall due to inflammation and scar tissue formation.
- Benign prostatic hyperplasia (BPH): An enlargement of the prostate gland, BPH can cause echogenic stroma due to tissue proliferation. The prostate may appear enlarged and echogenic on ultrasound.
- Prostatitis: Inflammation of the prostate, prostatitis can also lead to echogenic stroma due to inflammatory cell infiltration and tissue changes.
- Prostate cancer: A malignant tumor of the prostate, prostate cancer can present with echogenic stroma due to tumor growth and tissue alterations. However, further investigations are needed for definitive diagnosis.
- Fibrocystic changes: A common condition characterized by cysts and fibrous tissue in the breast, fibrocystic changes can cause echogenic stroma due to the increased fibrous tissue. The breast may appear dense and echogenic on ultrasound.
- Fibroadenomas: Benign tumors of the breast, fibroadenomas can appear echogenic on ultrasound due to their fibrous nature. They are usually well-defined and mobile.
- Breast cancer: A malignant tumor of the breast, breast cancer can also present with echogenic stroma, but further investigations are required for definitive diagnosis.
Echogenic Stroma in Different Organs
Echogenic stroma can be observed in various organs, and its appearance and significance can vary depending on the specific organ involved. Understanding the context of echogenic stroma within different organ systems is crucial for accurate diagnosis and appropriate management.
Echogenic Stroma in the Breast, What does echogenic stroma mean
Echogenic stroma in the breast is often observed on ultrasound imaging. The breast parenchyma, the tissue surrounding the ducts and lobules, can appear echogenic due to various factors.
- Expected Echogenicity: The breast parenchyma typically exhibits a heterogeneous echotexture with areas of both hyperechoic (bright) and hypoechoic (dark) regions. Echogenic stroma in the breast can present as focal or diffuse areas of increased echogenicity, often described as “dense” or “fibrotic” on ultrasound.
- Potential Causes: Echogenic stroma in the breast can be associated with several conditions, including:
- Fibrocystic changes: Common benign condition characterized by the presence of cysts and fibrous tissue.
- Fibroadenomas: Benign tumors composed of fibrous and glandular tissue.
- Breast cancer: In some cases, echogenic stroma can be a feature of breast cancer, particularly in dense breasts.
- Radiation therapy: Prior radiation therapy to the breast can lead to increased echogenicity of the stroma.
- Clinical Implications: The clinical significance of echogenic stroma in the breast depends on the specific findings and the patient’s clinical history. While it can be a benign finding, it is essential to consider the possibility of underlying pathology, particularly in the presence of other suspicious features. Further evaluation, such as biopsy, may be necessary to determine the cause of echogenic stroma in the breast.
Echogenic Stroma in the Uterus
Echogenic stroma in the uterus is often encountered during pelvic ultrasound examinations. The uterine stroma, the connective tissue surrounding the uterine muscle, can exhibit varying degrees of echogenicity.
- Expected Echogenicity: The uterine stroma typically appears as a hypoechoic (dark) zone surrounding the echogenic (bright) myometrium (uterine muscle). However, the echogenicity of the stroma can vary depending on the menstrual cycle phase, hormonal status, and other factors.
- Potential Causes: Echogenic stroma in the uterus can be associated with:
- Endometriosis: A condition where endometrial tissue grows outside the uterus, often leading to increased echogenicity of the stroma.
- Fibroids: Benign tumors of the uterine muscle that can cause increased echogenicity of the surrounding stroma.
- Adenomyosis: A condition where endometrial tissue invades the uterine muscle, resulting in increased echogenicity.
- Chronic inflammation: Inflammation of the uterine stroma can also lead to increased echogenicity.
- Clinical Implications: The presence of echogenic stroma in the uterus can be a sign of various conditions, some benign and others potentially requiring treatment. Further evaluation, including pelvic exams and imaging studies, may be necessary to determine the underlying cause and guide management strategies.
Echogenic Stroma in the Ovaries
Echogenic stroma in the ovaries is a common finding on ultrasound, and its appearance can vary significantly. The ovarian stroma, the connective tissue surrounding the follicles and other ovarian structures, can exhibit different echogenicities.
- Expected Echogenicity: The ovarian stroma typically appears as a hypoechoic (dark) zone surrounding the follicles and other ovarian structures. However, the echogenicity of the stroma can vary depending on the patient’s age, hormonal status, and other factors.
- Potential Causes: Echogenic stroma in the ovaries can be associated with:
- Polycystic ovary syndrome (PCOS): A hormonal disorder characterized by multiple cysts in the ovaries, often leading to increased echogenicity of the stroma.
- Ovarian cysts: Benign fluid-filled sacs in the ovary that can cause increased echogenicity of the surrounding stroma.
- Ovarian cancer: In some cases, echogenic stroma can be a feature of ovarian cancer, particularly in advanced stages.
- Ovarian aging: As women age, the ovarian stroma can become more echogenic due to the depletion of follicles and other changes.
- Clinical Implications: The presence of echogenic stroma in the ovaries can be a sign of various conditions, ranging from benign to potentially serious. Further evaluation, including pelvic exams and imaging studies, may be necessary to determine the underlying cause and guide management strategies.
Echogenic Stroma in the Prostate
Echogenic stroma in the prostate is a common finding on transrectal ultrasound (TRUS) examinations. The prostatic stroma, the connective tissue surrounding the glands and other prostatic structures, can exhibit varying degrees of echogenicity.
- Expected Echogenicity: The prostatic stroma typically appears as a hypoechoic (dark) zone surrounding the echogenic (bright) glandular tissue. However, the echogenicity of the stroma can vary depending on age, hormonal status, and other factors.
- Potential Causes: Echogenic stroma in the prostate can be associated with:
- Benign prostatic hyperplasia (BPH): A common condition characterized by an enlarged prostate, often leading to increased echogenicity of the stroma.
- Prostatitis: Inflammation of the prostate can cause increased echogenicity of the stroma.
- Prostate cancer: In some cases, echogenic stroma can be a feature of prostate cancer, particularly in advanced stages.
- Age-related changes: As men age, the prostatic stroma can become more echogenic due to the accumulation of fibrous tissue.
- Clinical Implications: The presence of echogenic stroma in the prostate can be a sign of various conditions, some benign and others potentially requiring treatment. Further evaluation, including TRUS-guided biopsies and other tests, may be necessary to determine the underlying cause and guide management strategies.
Echogenic Stroma in the Thyroid
Echogenic stroma in the thyroid is often observed on thyroid ultrasound examinations. The thyroid stroma, the connective tissue surrounding the thyroid follicles, can exhibit varying degrees of echogenicity.
- Expected Echogenicity: The thyroid stroma typically appears as a hypoechoic (dark) zone surrounding the echogenic (bright) thyroid follicles. However, the echogenicity of the stroma can vary depending on the patient’s age, hormonal status, and other factors.
- Potential Causes: Echogenic stroma in the thyroid can be associated with:
- Thyroiditis: Inflammation of the thyroid can cause increased echogenicity of the stroma.
- Nodules: Benign or malignant growths in the thyroid can cause increased echogenicity of the surrounding stroma.
- Hashimoto’s thyroiditis: An autoimmune disorder that affects the thyroid, often leading to increased echogenicity of the stroma.
- Age-related changes: As people age, the thyroid stroma can become more echogenic due to the accumulation of fibrous tissue.
- Clinical Implications: The presence of echogenic stroma in the thyroid can be a sign of various conditions, some benign and others potentially requiring treatment. Further evaluation, including thyroid function tests and biopsies, may be necessary to determine the underlying cause and guide management strategies.
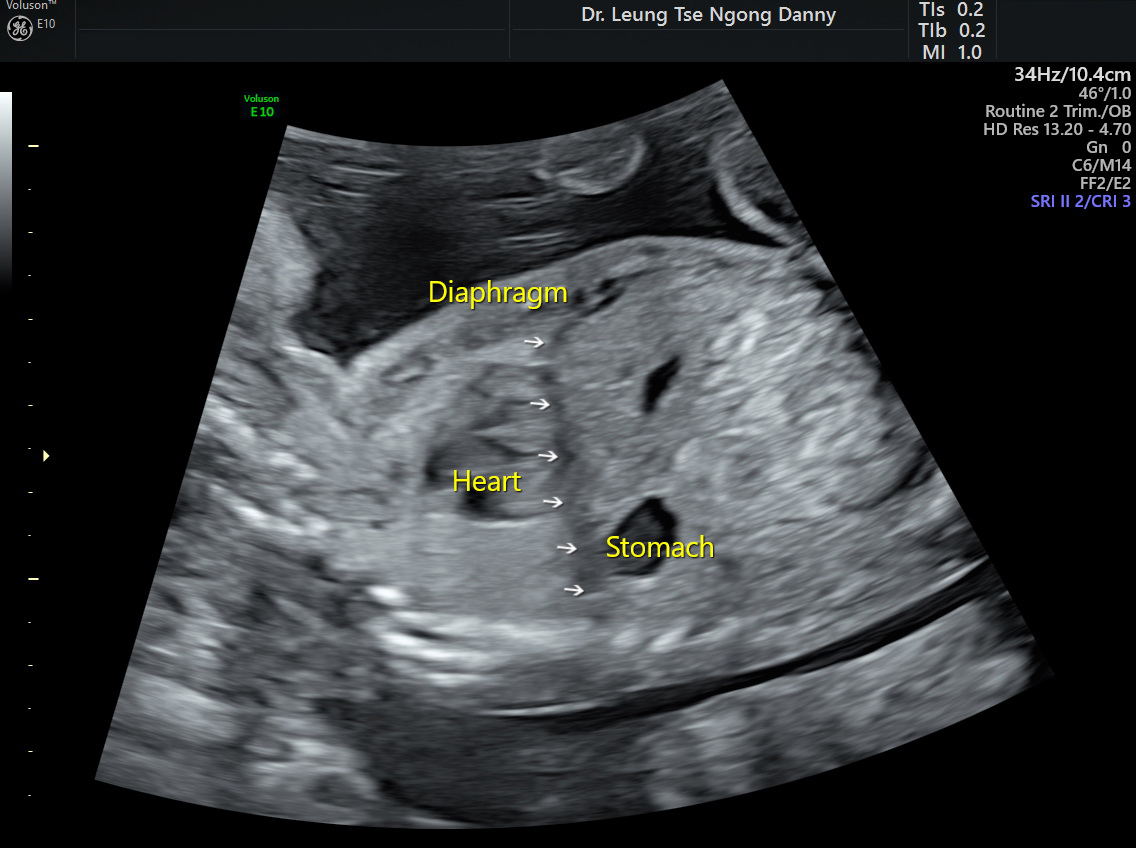
Echogenic Stroma in Pregnancy
Echogenic stroma, a bright, dense appearance on ultrasound, can sometimes be observed in various tissues during pregnancy. While it is not always a cause for concern, it can sometimes indicate potential issues that require further investigation and monitoring. Understanding the significance of echogenic stroma in pregnancy is crucial for accurate diagnosis and appropriate management.
Causes of Echogenic Stroma in Pregnancy
Echogenic stroma can be observed in different parts of the body during pregnancy, including the placenta, fetal tissues, and maternal organs. The causes can vary depending on the location and context.
- Placenta: Echogenic stroma in the placenta can be associated with several factors, including:
- Maternal age: Older mothers are more likely to have echogenic areas in the placenta.
- Multiple pregnancies: Placentas in multiple pregnancies often exhibit increased echogenicity.
- Placental abruption: This condition involves the separation of the placenta from the uterine wall, which can lead to echogenic areas in the placenta.
- Placental infarction: This occurs when a portion of the placenta loses its blood supply, resulting in echogenic areas.
- Chronic villitis: This is an inflammation of the placental villi, which can cause echogenic areas.
- Fetal tissues: Echogenic stroma in fetal tissues can be observed in:
- Fetal kidneys: Echogenic foci in the fetal kidneys can be associated with various conditions, including:
- Benign cysts: These are often small and do not cause any harm.
- Urinary tract infections: Infections can cause inflammation and echogenic areas in the kidneys.
- Obstructive uropathy: Blockage of the urinary tract can lead to kidney enlargement and echogenic areas.
- Fetal heart: Echogenic foci in the fetal heart can be associated with:
- Benign fibromas: These are non-cancerous tumors that can cause echogenic areas in the heart.
- Congenital heart defects: Certain heart defects can cause echogenic areas in the heart.
- Fetal brain: Echogenic foci in the fetal brain can be associated with:
- Periventricular leukomalacia: This is a brain injury that can occur in premature infants, causing echogenic areas.
- Cerebral hemorrhage: Bleeding in the brain can also lead to echogenic areas.
- Fetal kidneys: Echogenic foci in the fetal kidneys can be associated with various conditions, including:
- Maternal organs: Echogenic stroma in maternal organs can be associated with:
- Uterus: Echogenic areas in the uterine wall can be associated with:
- Fibroids: These are non-cancerous growths that can cause echogenic areas in the uterus.
- Adenomyosis: This is a condition where the lining of the uterus grows into the uterine wall, causing echogenic areas.
- Ovaries: Echogenic areas in the ovaries can be associated with:
- Cysts: These are fluid-filled sacs that can cause echogenic areas in the ovaries.
- Ovarian tumors: Some ovarian tumors can be echogenic.
- Uterus: Echogenic areas in the uterine wall can be associated with:
Echogenic Stroma: Diagnostic and Therapeutic Considerations
Echogenic stroma, a finding often observed during ultrasound examinations, can be a sign of various underlying conditions. Understanding the diagnostic tools and therapeutic approaches associated with echogenic stroma is crucial for accurate diagnosis and effective management.
Diagnostic Tools and Procedures
Investigating echogenic stroma involves a multi-faceted approach that often includes a combination of diagnostic tools and procedures. These tools help healthcare professionals visualize the affected area, understand the underlying cause, and guide treatment decisions.
- Ultrasound Imaging: This non-invasive technique uses sound waves to create images of internal structures. Ultrasound is often the initial diagnostic tool used to detect echogenic stroma. It provides valuable information about the size, shape, and texture of the affected area.
- Magnetic Resonance Imaging (MRI): MRI utilizes magnetic fields and radio waves to produce detailed images of soft tissues. It can provide more detailed information about the structure and composition of echogenic stroma compared to ultrasound, especially in complex cases.
- Biopsy: In some cases, a biopsy may be necessary to obtain a tissue sample for microscopic examination. This helps confirm the diagnosis and determine the underlying cause of the echogenic stroma.
- Blood Tests: Blood tests can be used to assess overall health, identify potential underlying conditions, and monitor treatment response.
Therapeutic Approaches
Treatment for conditions associated with echogenic stroma varies depending on the underlying cause, severity, and location of the echogenic stroma.
- Medications: In some cases, medications may be prescribed to manage symptoms or address the underlying cause of the echogenic stroma. For example, antibiotics may be used to treat infections, while hormone therapy may be used to manage conditions related to hormonal imbalances.
- Surgery: Surgical intervention may be necessary in certain cases, such as when the echogenic stroma is causing pain, obstruction, or other complications. For instance, surgery may be required to remove a tumor or cyst associated with echogenic stroma.
- Other Interventions: Depending on the specific condition, other interventions may be used, such as radiation therapy or chemotherapy.
Examples of Treatment Options
- Fibroids: Treatment options for uterine fibroids associated with echogenic stroma may include medications such as gonadotropin-releasing hormone (GnRH) agonists, selective estrogen receptor modulators (SERMs), or nonsteroidal anti-inflammatory drugs (NSAIDs). Surgical options include myomectomy (removal of fibroids) or hysterectomy (removal of the uterus).
- Ovarian Cysts: Treatment for ovarian cysts associated with echogenic stroma often involves monitoring the cyst over time to see if it resolves on its own. If the cyst is large, causing symptoms, or suspicious for malignancy, surgery may be recommended.
- Prostate Enlargement: Treatment for prostate enlargement associated with echogenic stroma may include medications such as alpha-blockers or 5-alpha reductase inhibitors. In severe cases, surgery may be necessary.
Research and Future Directions: What Does Echogenic Stroma Mean
Research on echogenic stroma is an active area of investigation, with ongoing efforts to understand its causes, refine diagnostic techniques, and develop targeted treatment strategies. The focus is on unraveling the intricate mechanisms underlying echogenic stroma formation, improving its detection and characterization, and ultimately, improving patient outcomes.
Understanding the Mechanisms of Echogenic Stroma Formation
The precise mechanisms behind echogenic stroma development are not fully understood. Current research is exploring various contributing factors, including:
- Cellular and Molecular Changes: Investigating alterations in cellular composition, proliferation, and apoptosis within the stroma. Studies are examining the role of specific genes and proteins involved in these processes. For example, research is focusing on the expression of collagen, elastin, and other extracellular matrix components in echogenic stroma.
- Microenvironment: Exploring the influence of the microenvironment surrounding the stroma, including vascularization, oxygen levels, and the presence of inflammatory mediators. Studies are analyzing the role of growth factors, cytokines, and chemokines in echogenic stroma formation.
- Genetic and Epigenetic Factors: Examining the potential role of genetic mutations and epigenetic modifications in predisposing individuals to echogenic stroma. Research is exploring the contribution of specific genetic variants and altered gene expression patterns in the development of echogenic stroma.
Improving Diagnostic Accuracy and Characterization
Advances in ultrasound technology and image analysis techniques are enhancing the ability to detect and characterize echogenic stroma.
- High-Resolution Ultrasound: The use of high-frequency transducers and advanced imaging modes, such as harmonic imaging and elastography, provides improved resolution and tissue characterization, enabling more precise identification of echogenic stroma.
- Quantitative Ultrasound: Research is exploring the application of quantitative ultrasound parameters, such as echogenicity measurements and texture analysis, to differentiate echogenic stroma from other tissue types. This may improve diagnostic accuracy and facilitate early detection.
- Artificial Intelligence: Machine learning algorithms are being developed to analyze ultrasound images and identify patterns associated with echogenic stroma. This could potentially improve the speed and accuracy of diagnosis.
Developing Targeted Therapeutic Strategies
The development of targeted therapies for conditions associated with echogenic stroma is an emerging area of research.
- Anti-Fibrotic Therapies: Research is exploring the use of anti-fibrotic drugs, which target the excessive production of collagen and other extracellular matrix components, to reduce the size and density of echogenic stroma.
- Immunomodulatory Therapies: Investigating the role of immune system modulation in influencing echogenic stroma formation. Therapies targeting specific immune cells or pathways may hold potential for reducing inflammation and fibrosis.
- Personalized Medicine: Understanding the genetic and molecular basis of echogenic stroma may enable the development of personalized treatment strategies tailored to individual patient characteristics. This approach could potentially improve treatment effectiveness and minimize adverse effects.
Echogenic stroma is a complex topic that often sparks curiosity in both patients and medical professionals. While it can be a sign of something serious, it’s important to remember that it’s not always a cause for concern. By understanding the different causes and implications of echogenic stroma, we can better navigate the world of medical imaging and make informed decisions about our health.
FAQ Section
Is echogenic stroma always a sign of something bad?
No, echogenic stroma isn’t always a sign of something bad. Sometimes it’s simply a normal variation in tissue. However, it can also be a sign of a medical condition, so it’s important to discuss any findings with your doctor.
What are some common causes of echogenic stroma?
Some common causes of echogenic stroma include inflammation, infection, fibrosis, and tumors. However, the specific cause will vary depending on the location of the echogenic stroma.
How is echogenic stroma diagnosed?
Echogenic stroma is typically diagnosed using ultrasound imaging. In some cases, additional tests, such as a biopsy, may be necessary to determine the cause.
What are the treatment options for echogenic stroma?
The treatment options for echogenic stroma will vary depending on the underlying cause. In some cases, no treatment may be necessary. In other cases, treatment may include medications, surgery, or other interventions.






