What is fibromuscular stroma fistula –
What is fibromuscular stroma fistula? This intriguing question leads us into the realm of rare medical conditions, specifically focusing on a fistula within the fibromuscular stroma, a crucial component of various organs and tissues. While this condition may not be widely known, its impact on affected individuals is significant, prompting us to delve into its intricacies.
Fibromuscular stroma fistula, often referred to as a “fistula,” involves an abnormal connection between the fibromuscular stroma and another structure, such as a blood vessel or an organ. This connection can disrupt the normal function of the affected tissues, leading to a range of symptoms and complications. Understanding the anatomy and physiology of the fibromuscular stroma is essential to grasp the implications of this fistula.
*
Fibromuscular Stroma Fistula
Fibromuscular stroma fistula (FMSF) is a rare but potentially serious condition that occurs when there is an abnormal connection between the blood vessels and the fibromuscular stroma of an organ. This connection allows blood to leak from the vessels into the surrounding tissue, leading to a variety of symptoms depending on the location and severity of the fistula.
Definition and Background
Fibromuscular stroma fistula is characterized by an abnormal connection between the blood vessels and the fibromuscular stroma of an organ. The fibromuscular stroma is the supporting tissue of an organ, made up of fibrous connective tissue and smooth muscle cells. In FMSF, this supporting tissue becomes abnormally vascularized, with blood vessels growing into and through it. This can lead to a leak of blood from the vessels into the surrounding tissue, creating a fistula.The exact cause of FMSF is unknown, but it is thought to be a combination of genetic and environmental factors.
Some researchers believe that it may be triggered by trauma, infection, or inflammation.
Historical Overview
The first documented case of FMSF was reported in 1976 in a patient with uterine fibroids. Since then, FMSF has been identified in a variety of organs, including the kidneys, liver, spleen, and pancreas. However, the condition remains relatively rare and poorly understood.Early research focused on understanding the pathological processes involved in FMSF. The development of advanced imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, has significantly improved the diagnosis and understanding of this condition.
Prevalence and Incidence
The prevalence and incidence of FMSF are difficult to determine due to the rarity of the condition. However, it is estimated that FMSF affects approximately 1 in 10,000 people. The incidence of FMSF varies depending on the organ affected. For example, FMSF is more common in the kidneys than in other organs. It is also more common in women than in men, likely due to the higher incidence of uterine fibroids in women.
Anatomy and Physiology of the Fibromuscular Stroma
The fibromuscular stroma is a vital component of many organs and tissues, providing structural support and contributing to essential physiological functions. Understanding its anatomy and physiology is crucial for comprehending the potential impact of fibromuscular stroma fistula on organ function.
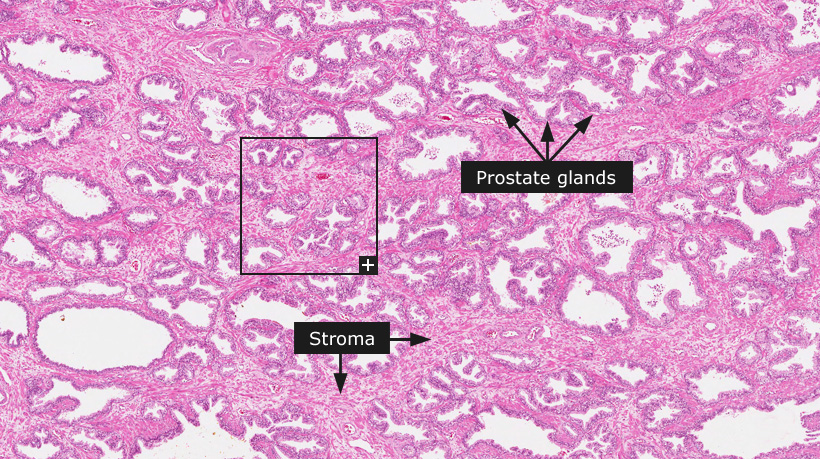
Location and Cellular Composition
The fibromuscular stroma is found in various organs, including the kidneys, liver, spleen, and lymph nodes. It is located beneath the epithelial lining and surrounds the functional parenchyma, the tissue responsible for the organ’s primary function. The fibromuscular stroma is composed of a complex network of connective tissue, including:
- Fibroblasts: These cells produce and maintain the extracellular matrix, providing structural support.
- Smooth muscle cells: These cells contract and relax, contributing to organ function and regulating blood flow.
- Blood vessels: These vessels supply the stroma with nutrients and oxygen and remove waste products.
- Extracellular matrix: This complex network of proteins and polysaccharides provides structural support and facilitates cell-to-cell communication.
Physiological Functions
The fibromuscular stroma plays a crucial role in supporting organ function by:
- Structural support: The stroma provides a framework for the organ, helping to maintain its shape and integrity.
- Regulation of blood flow: Smooth muscle cells in the stroma can contract and relax, regulating blood flow to the organ and ensuring adequate oxygen and nutrient delivery.
- Immune defense: The stroma contains immune cells that help protect the organ from infection and injury.
- Tissue repair: Fibroblasts in the stroma play a vital role in wound healing and tissue regeneration.
- Organ development: The stroma provides a scaffold for organ development, guiding the growth and differentiation of cells.
Impact of Fibromuscular Stroma Fistula on Organ Function
A fibromuscular stroma fistula is an abnormal connection between the stroma and another structure, such as a blood vessel or a hollow organ. This can disrupt the normal function of the stroma, leading to various complications, including:
- Bleeding: A fistula can allow blood to leak from a blood vessel into the stroma, leading to internal bleeding.
- Infection: A fistula can provide a pathway for bacteria to enter the stroma, leading to infection.
- Organ dysfunction: The disruption of the stroma’s structural integrity and physiological functions can impair organ function.
- Scarring: Chronic inflammation and tissue damage associated with a fistula can lead to scarring, further compromising organ function.
Causes and Risk Factors of Fibromuscular Stroma Fistula
While the exact causes of fibromuscular stroma fistula (FMSF) are not fully understood, researchers have identified several potential contributing factors, including genetic predisposition and environmental influences. Understanding the causes and risk factors is crucial for early detection, prevention, and management of FMSF. This knowledge allows for personalized interventions and targeted therapies to improve patient outcomes.
Genetic Predisposition
Genetic factors play a significant role in the development of FMSF. Family history of FMSF is a major risk factor, suggesting a genetic component. Researchers are actively investigating specific genes that may increase susceptibility to FMSF. While these studies are ongoing, some genes involved in immune system regulation, tissue development, and connective tissue formation are being examined as potential contributors.
Environmental Factors
Environmental factors can also influence the development of FMSF. These include:
- Exposure to certain chemicals: Exposure to industrial chemicals or toxins may contribute to the development of FMSF in some individuals. While research is ongoing, some chemicals are suspected to interfere with tissue repair and immune responses, potentially leading to fistula formation.
- Infections: Certain infections, particularly those affecting the gastrointestinal tract, have been linked to FMSF. These infections may trigger an inflammatory response that damages the fibromuscular stroma, creating an environment conducive to fistula formation.
- Trauma: Physical trauma, such as surgical procedures or injuries, can disrupt the integrity of the fibromuscular stroma and increase the risk of fistula formation.
- Lifestyle factors: Certain lifestyle factors, such as smoking, alcohol consumption, and a sedentary lifestyle, can contribute to chronic inflammation and weakened tissue integrity, increasing the risk of FMSF.
Risk Factors in Different Organs and Tissues
The causes and risk factors of FMSF can vary depending on the specific organ or tissue involved. For example:
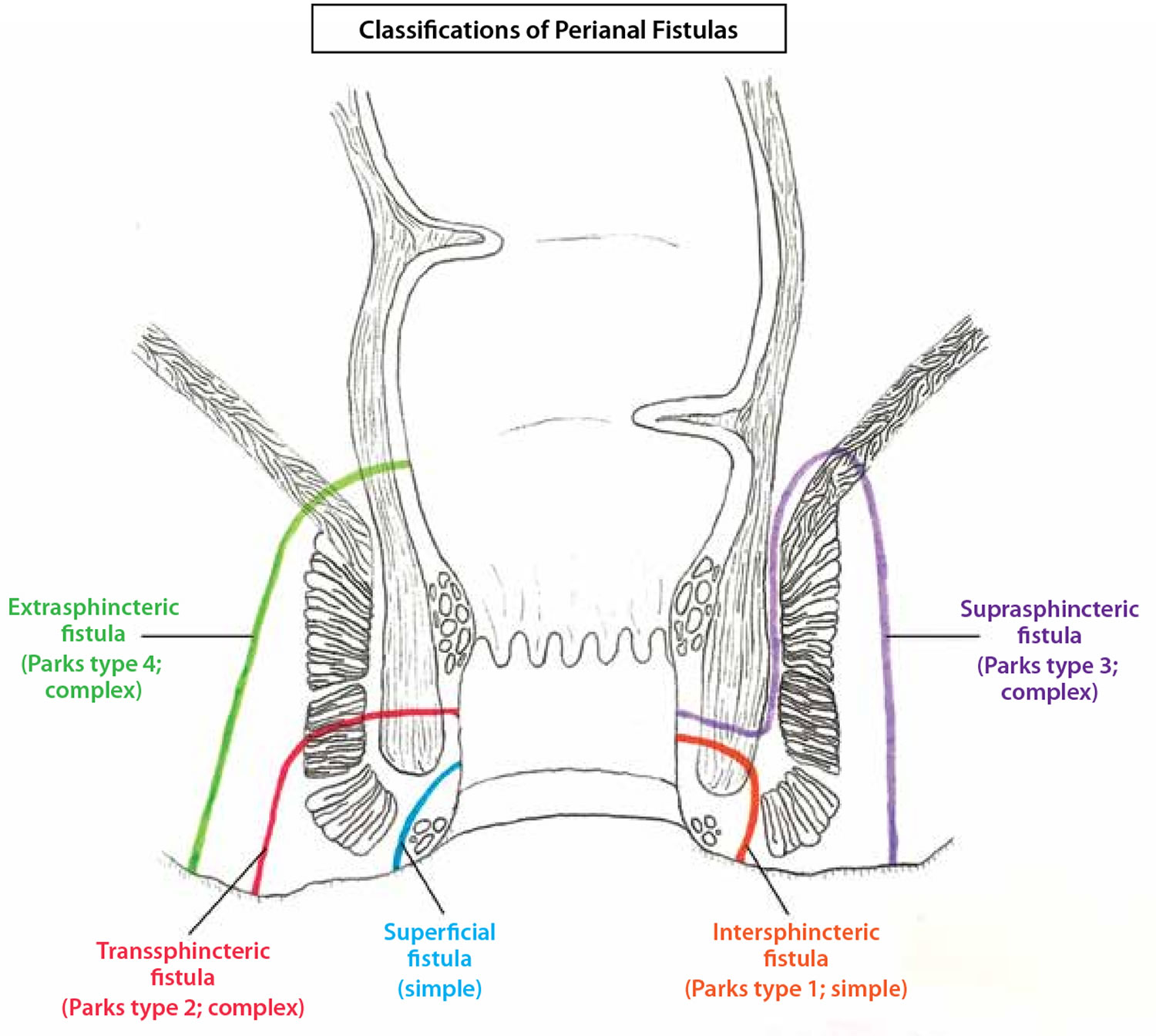
- Gastrointestinal Tract: FMSF in the gastrointestinal tract is often associated with inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis. These conditions cause chronic inflammation and damage to the intestinal wall, increasing the risk of fistula formation.
- Genitourinary Tract: FMSF in the genitourinary tract can be associated with pelvic inflammatory disease (PID), endometriosis, and surgical procedures. PID causes inflammation in the reproductive organs, while endometriosis can lead to tissue growth and adhesions, both of which can increase the risk of fistula formation.
- Skin: FMSF in the skin is often associated with trauma, infection, and inflammatory conditions like hidradenitis suppurativa. These conditions can disrupt the integrity of the skin and underlying tissues, leading to fistula formation.
Symptoms and Diagnosis of Fibromuscular Stroma Fistula
Fibromuscular stroma fistula (FMSF) is a rare condition that can cause a variety of symptoms, depending on the location and severity of the fistula. The symptoms are often subtle and may be mistaken for other conditions. Therefore, it is crucial to be aware of the potential signs and seek prompt medical attention if you suspect you might have an FMSF.
Symptoms of Fibromuscular Stroma Fistula
The symptoms of FMSF can vary depending on the location and severity of the fistula. Common symptoms include:
- Pain: This is a common symptom, and it can be localized to the area of the fistula or more widespread. The pain can be sharp, dull, or aching, and it may worsen with activity.
- Swelling: Swelling in the affected area is another common symptom. The swelling may be noticeable or subtle, and it may fluctuate in size.
- Redness: Redness in the affected area is a sign of inflammation and may be accompanied by warmth.
- Discharge: A discharge from the fistula may be present, and it can be clear, cloudy, or bloody. The discharge may be intermittent or continuous.
- Fever: A fever is a sign of infection, and it may be present if the fistula is infected.
- Weakness: Weakness in the affected area can occur due to the disruption of normal tissue function caused by the fistula.
- Numbness: Numbness or tingling in the affected area can also occur due to the disruption of nerve function caused by the fistula.
Diagnosis of Fibromuscular Stroma Fistula
Diagnosing FMSF can be challenging due to its rarity and the variety of symptoms that can be present. However, a thorough medical history and physical examination, combined with appropriate imaging techniques and biopsies, can help confirm the diagnosis.
Imaging Techniques
- Ultrasound: Ultrasound is a non-invasive imaging technique that uses sound waves to create images of the inside of the body. It is often the first-line imaging technique used to diagnose FMSF. Ultrasound can help identify the fistula, its location, and its size.
- Magnetic Resonance Imaging (MRI): MRI is another non-invasive imaging technique that uses magnetic fields and radio waves to create detailed images of the inside of the body. MRI can provide more detailed images of the fistula than ultrasound, and it can also help assess the extent of the surrounding tissue involvement.
- Computed Tomography (CT) Scan: CT scans use X-rays to create cross-sectional images of the body. CT scans can be helpful in diagnosing FMSF, especially if the fistula is located in a complex area of the body.
Biopsy
A biopsy is a procedure in which a small sample of tissue is removed from the body and examined under a microscope. A biopsy can help confirm the diagnosis of FMSF and determine the type of tissue involved in the fistula.
Clinical Cases
- A 35-year-old woman presented with a history of pain and swelling in her right breast. Ultrasound examination revealed a fistula between the fibromuscular stroma and the ductal system. A biopsy confirmed the diagnosis of FMSF.
- A 50-year-old man presented with a history of pain and swelling in his left testicle. MRI revealed a fistula between the fibromuscular stroma and the epididymis. A biopsy confirmed the diagnosis of FMSF.
Treatment Options for Fibromuscular Stroma Fistula
Treating fibromuscular stroma fistula is crucial to prevent complications like infections, pain, and tissue damage. The treatment approach depends on the severity of the fistula, its location, and the patient’s overall health.
Surgical Interventions
Surgical intervention is often the primary treatment for fibromuscular stroma fistulas. The goal of surgery is to close the fistula and prevent further fluid leakage. Here are the common surgical procedures:
- Fistulectomy: This involves surgically removing the fistula and surrounding tissue. It’s effective for small, localized fistulas. However, it can be challenging in cases where the fistula is deep or close to vital structures.
- Fistula ligation: This procedure involves tying off the fistula with sutures. It’s a simpler and less invasive approach compared to fistulectomy. However, it might not be effective for larger fistulas or those with complex anatomy.
- Fistula repair: This technique involves closing the fistula using sutures or tissue grafts. It’s a more complex procedure but can be effective for larger and more complex fistulas.
Medical Management
In some cases, medical management might be considered as an alternative or complementary treatment to surgery. Medical management focuses on controlling symptoms and reducing the risk of complications.
- Antibiotics: Antibiotics are prescribed to prevent or treat infections associated with the fistula. They are particularly important in cases where the fistula is draining pus or other fluids.
- Anti-inflammatory medications: These medications can help reduce inflammation and pain around the fistula.
- Drainage: In some cases, draining the fistula can help reduce pressure and promote healing. This can be achieved through a small incision or by inserting a drain tube.
Comparison of Treatment Options, What is fibromuscular stroma fistula
Here’s a table summarizing the benefits and drawbacks of different treatment options for fibromuscular stroma fistula:
| Treatment Option | Benefits | Drawbacks |
|---|---|---|
| Surgical Interventions | Effective for most fistulas, can permanently close the fistula | Risk of complications like infection, bleeding, and scarring, may require a lengthy recovery period |
| Medical Management | Less invasive, can be effective for managing symptoms | May not permanently close the fistula, may not be effective for all types of fistulas |
Prognosis and Long-Term Management: What Is Fibromuscular Stroma Fistula
The prognosis for individuals with fibromuscular stroma fistula varies depending on several factors, including the location and severity of the fistula, the patient’s overall health, and the effectiveness of treatment. While some cases resolve spontaneously or with conservative management, others require surgical intervention or long-term monitoring.
Prognosis
The prognosis for fibromuscular stroma fistula depends on several factors, including:
- Location: Fistulas located in the upper gastrointestinal tract (e.g., esophagus, stomach) are generally considered more serious than those in the lower gastrointestinal tract (e.g., colon, rectum). This is because fistulas in the upper GI tract can lead to more severe complications, such as bleeding, malnutrition, and sepsis.
- Severity: The size and complexity of the fistula can influence the prognosis. Larger and more complex fistulas may be more difficult to treat and have a higher risk of complications.
- Underlying Medical Conditions: Patients with other medical conditions, such as diabetes, autoimmune disorders, or cancer, may have a poorer prognosis.
- Treatment Response: The effectiveness of treatment, whether conservative or surgical, plays a crucial role in determining the prognosis.
Long-Term Management
Long-term management of fibromuscular stroma fistula focuses on preventing complications, monitoring the condition, and improving quality of life.
- Monitoring: Regular follow-up appointments with a healthcare professional are essential to monitor the fistula and detect any signs of complications. This may involve physical examinations, imaging studies (e.g., endoscopy, CT scan), and laboratory tests (e.g., blood work).
- Lifestyle Modifications: Lifestyle modifications, such as a balanced diet, regular exercise, and stress management, can contribute to overall health and may help prevent complications.
- Medications: Depending on the underlying cause and symptoms, medications may be prescribed to manage pain, infection, or other associated conditions.
- Surgery: In some cases, surgery may be necessary to repair the fistula, remove the underlying cause, or manage complications.
Patient Guide
Here’s a guide for patients to effectively manage their fibromuscular stroma fistula:
- Understand Your Condition: Learn about the nature of your fistula, its potential complications, and available treatment options.
- Follow Up Regularly: Attend all scheduled appointments with your healthcare provider to monitor your condition and discuss any concerns.
- Maintain a Healthy Lifestyle: Eat a balanced diet, exercise regularly, and manage stress to support your overall health.
- Report Any Changes: Contact your healthcare provider immediately if you experience any new or worsening symptoms, such as fever, pain, bleeding, or changes in bowel habits.
- Ask Questions: Don’t hesitate to ask your healthcare provider any questions you may have about your condition, treatment, or long-term management.
Research and Future Directions

While significant progress has been made in understanding fibromuscular stroma fistula (FMSF), there are still many unanswered questions and areas for future research. This research is crucial to improve diagnosis, treatment, and ultimately, the long-term outcomes for patients with FMSF.
Current Research Gaps and Future Investigations
The current understanding of FMSF is still evolving, and further research is needed to address several critical areas.
- The exact pathogenesis of FMSF: While the role of inflammation and immune dysregulation is suspected, the precise mechanisms that lead to the formation of fistulas remain unclear. More research is needed to elucidate the cellular and molecular events involved in FMSF development.
- The natural history of FMSF: Longitudinal studies are required to understand the progression of FMSF over time, including the factors that influence its severity and the likelihood of complications. This information will be vital for developing personalized treatment strategies.
- The role of genetics in FMSF: Family history suggests a possible genetic predisposition to FMSF. Genetic studies are needed to identify potential susceptibility genes and their influence on the development and progression of FMSF.
- The efficacy of different treatment approaches: Clinical trials are needed to compare the effectiveness of various treatment modalities, including surgical intervention, minimally invasive techniques, and medical management. This will help optimize treatment strategies based on individual patient characteristics and the severity of the fistula.
Development of New Diagnostic Tools
The development of novel diagnostic tools is essential for early detection and accurate diagnosis of FMSF. Current diagnostic methods often rely on invasive procedures, such as biopsies and imaging studies. Research efforts should focus on developing non-invasive or minimally invasive diagnostic techniques that are sensitive, specific, and readily available.
- Advanced imaging techniques: Further development and refinement of imaging techniques like magnetic resonance imaging (MRI) and computed tomography (CT) with contrast agents could improve the detection of FMSF and provide more detailed information about the anatomy and extent of the fistula.
- Biomarkers for FMSF: Identifying specific biomarkers in blood or other bodily fluids that are associated with FMSF could facilitate early detection and diagnosis. Research into potential biomarkers, such as inflammatory markers or proteins associated with tissue damage, is crucial.
- Molecular diagnostics: Exploring the use of molecular diagnostics, such as gene expression profiling or proteomic analysis, may provide valuable insights into the molecular mechanisms underlying FMSF and aid in personalized diagnosis and treatment.
Development of New Treatment Approaches
The development of new treatment approaches for FMSF is a priority, particularly those that are minimally invasive, effective, and have fewer side effects.
- Targeted therapies: Research into targeted therapies that specifically address the underlying mechanisms of FMSF, such as inflammation or immune dysregulation, could offer more effective and less invasive treatment options.
- Tissue engineering and regenerative medicine: Exploring the potential of tissue engineering and regenerative medicine to repair damaged tissues and restore normal function in patients with FMSF is a promising area of research. This could involve the development of biocompatible materials or the use of stem cells to promote tissue regeneration.
- Minimally invasive surgical techniques: Further development of minimally invasive surgical techniques, such as endoscopic or laparoscopic procedures, could reduce the risk of complications and improve recovery time for patients with FMSF.
Unanswered Questions and Research Priorities
To advance the understanding and management of FMSF, several critical research questions remain unanswered.
- What are the long-term consequences of FMSF, and how do they vary depending on the location and severity of the fistula?
- What factors contribute to the development of complications associated with FMSF, such as infection, bleeding, or obstruction?
- Can we develop predictive models to identify patients at higher risk for developing FMSF or experiencing complications?
- What are the optimal treatment strategies for different types and stages of FMSF?
- How can we improve the quality of life for patients with FMSF and reduce the impact of the condition on their daily lives?
Fibromuscular stroma fistula is a complex condition requiring careful diagnosis and management. While research continues to uncover more about this rare condition, advancements in diagnostic tools and treatment options offer hope for individuals facing its challenges. By understanding the causes, symptoms, and treatment approaches, we can contribute to a more informed approach to managing this condition and improving patient outcomes.
Essential Questionnaire
What are the most common symptoms of fibromuscular stroma fistula?
Symptoms vary depending on the location of the fistula. Common symptoms include pain, swelling, bleeding, and dysfunction of the affected organ.
Is fibromuscular stroma fistula always a serious condition?
The severity of fibromuscular stroma fistula depends on its location, size, and the presence of complications. Some fistulas may be relatively benign, while others can lead to life-threatening conditions.
What are the long-term implications of fibromuscular stroma fistula?
Long-term implications can vary depending on the individual and the condition’s management. Individuals with fibromuscular stroma fistula often require ongoing monitoring and may experience complications in the future.
-*






+%5Bglib%5D.jpg?w=700)