What is the fibromuscular stroma of the prostate? This intricate network of tissues, residing within the prostate gland, plays a crucial role in both prostate function and health. It’s a dynamic environment composed of specialized cells, a complex extracellular matrix, and intricate interactions that contribute to the gland’s development, growth, and overall function.
The fibromuscular stroma provides structural support, influences urine flow and sperm transport, and plays a critical role in prostate health by contributing to the gland’s normal development and growth. However, alterations in the stroma’s composition and function can contribute to various prostate disorders, such as benign prostatic hyperplasia (BPH) and prostate cancer.
Introduction to the Fibromuscular Stroma of the Prostate

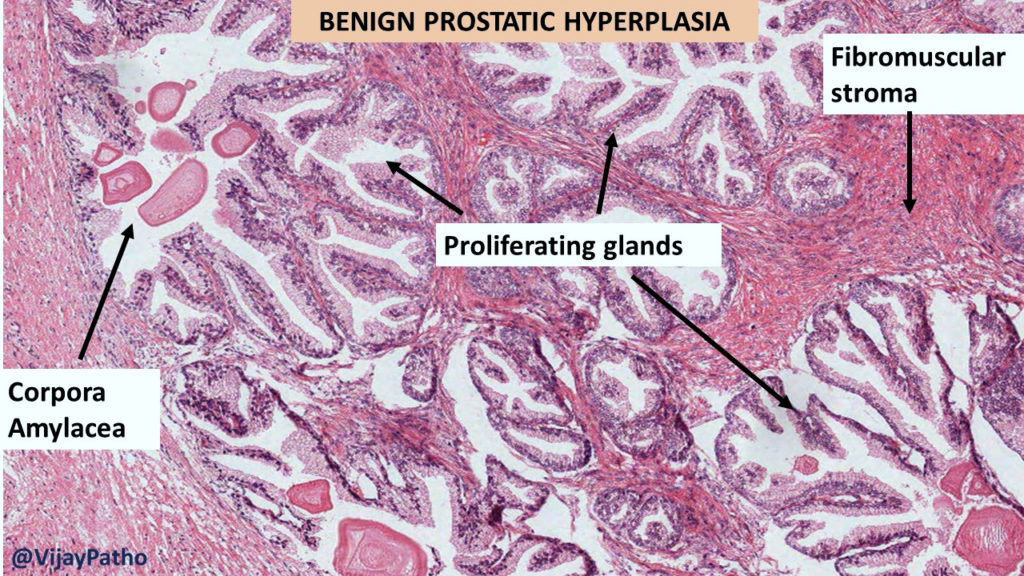
The fibromuscular stroma of the prostate is a dense, connective tissue framework that provides structural support and plays a critical role in the gland’s function. It is located throughout the prostate gland, surrounding the epithelial cells that line the glands and ducts.The fibromuscular stroma is essential for maintaining the shape and integrity of the prostate. It also contributes to the regulation of prostate growth and development, as well as the movement of secretions through the gland.
Cellular Components of the Fibromuscular Stroma
The fibromuscular stroma is composed of a variety of cell types, including:
- Fibroblasts: These cells are responsible for producing the extracellular matrix, which provides structural support and allows for the diffusion of nutrients and waste products.
- Smooth muscle cells: These cells are responsible for the contraction and relaxation of the stroma, which helps to regulate the flow of prostatic secretions.
- Endothelial cells: These cells line the blood vessels within the stroma, facilitating the exchange of oxygen, nutrients, and waste products.
- Immune cells: The stroma contains various immune cells, such as macrophages and lymphocytes, which play a role in the defense against infection and inflammation.
Cellular Composition of the Fibromuscular Stroma
The fibromuscular stroma of the prostate is a complex and dynamic tissue, playing a crucial role in supporting the glandular epithelium and maintaining prostate function. It is composed of a diverse population of cells, each contributing to the unique properties of this tissue.
Types of Cells
Understanding the different cell types within the fibromuscular stroma is essential for comprehending its structure and function. The main cell types include smooth muscle cells, fibroblasts, and other connective tissue cells.
- Smooth Muscle Cells: These elongated, spindle-shaped cells are responsible for the contractile properties of the stroma. They are arranged in bundles and sheets, providing support and facilitating the movement of fluids and secretions within the prostate. Smooth muscle cells are regulated by neurotransmitters and hormones, contributing to the complex regulation of prostate function.
- Fibroblasts: These cells are the primary producers of the extracellular matrix (ECM), which provides structural support and acts as a scaffold for other cells within the stroma. Fibroblasts synthesize collagen, elastin, and other ECM components, contributing to the tissue’s elasticity and resilience.
- Other Connective Tissue Cells: The fibromuscular stroma also contains other connective tissue cells, including mast cells, macrophages, and lymphocytes. These cells play important roles in immune defense, tissue repair, and inflammation. For example, mast cells release histamine and other mediators involved in allergic reactions and inflammation, while macrophages engulf and digest cellular debris and pathogens, contributing to tissue homeostasis.
Roles of Cell Types
Each cell type within the fibromuscular stroma contributes to its overall function and structure.
- Smooth Muscle Cells: The contractile nature of smooth muscle cells allows for the regulation of prostatic fluid flow and the expulsion of semen during ejaculation. Their contraction also influences the pressure within the prostate, contributing to the regulation of glandular secretion.
- Fibroblasts: Fibroblasts are responsible for maintaining the integrity and organization of the ECM, providing structural support and creating a suitable environment for other cell types. The ECM also plays a role in cell signaling and communication, influencing the behavior of other cells within the stroma.
- Other Connective Tissue Cells: The presence of immune cells within the fibromuscular stroma is essential for maintaining tissue homeostasis and responding to infection or injury. These cells contribute to the immune surveillance of the prostate, protecting it from pathogens and promoting tissue repair.
Interactions Between Cell Types
The different cell types within the fibromuscular stroma interact in complex ways, influencing each other’s behavior and contributing to the overall function of the tissue.
- Smooth Muscle Cells and Fibroblasts: These cells interact through direct contact and through the ECM. Fibroblasts produce ECM components that provide a scaffold for smooth muscle cells, guiding their arrangement and influencing their contractile activity. Smooth muscle cells, in turn, release factors that regulate fibroblast activity, influencing ECM production and remodeling.
- Fibroblasts and Immune Cells: Fibroblasts play a role in regulating immune responses within the stroma. They can release chemokines and cytokines that attract immune cells to the site of inflammation or injury. Immune cells, in turn, can influence fibroblast activity, promoting tissue repair and remodeling.
- Smooth Muscle Cells and Immune Cells: Smooth muscle cells can also interact with immune cells, contributing to the regulation of inflammation and tissue repair. For example, smooth muscle cells can release factors that suppress immune responses, helping to maintain tissue homeostasis.
Clinical Significance of the Fibromuscular Stroma: What Is The Fibromuscular Stroma Of The Prostate
The fibromuscular stroma is not just a passive scaffold within the prostate; it actively participates in the gland’s physiology and pathology. Its intricate structure and cellular composition play crucial roles in normal prostate function, and alterations within the stroma can significantly impact prostate health, leading to various clinical conditions.
Role of the Fibromuscular Stroma in Prostate Pathologies
The fibromuscular stroma’s involvement in prostate pathologies is multifaceted, influencing the development and progression of conditions like benign prostatic hyperplasia (BPH), prostate cancer, and prostatitis.
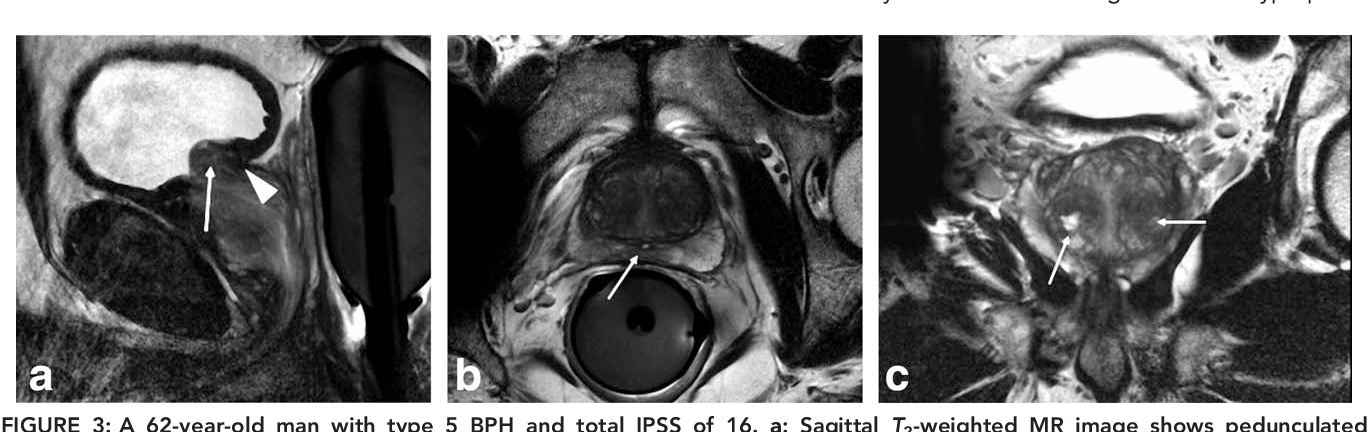
- Benign Prostatic Hyperplasia (BPH): BPH is characterized by an enlargement of the prostate gland, primarily due to an increase in stromal cells and smooth muscle. The fibromuscular stroma undergoes significant changes in BPH, including hyperplasia, hypertrophy, and fibrosis. These changes contribute to the compression of the urethra, leading to urinary symptoms such as difficulty urinating, frequent urination, and urinary retention.
- Prostate Cancer: The fibromuscular stroma interacts with prostate cancer cells in complex ways. Stromal cells can either promote or inhibit tumor growth. For example, stromal cells can secrete growth factors that stimulate tumor cell proliferation. Conversely, they can also produce factors that suppress tumor growth. Additionally, the stromal microenvironment can influence the spread of prostate cancer, creating a conducive environment for metastasis.
- Prostatitis: Prostatitis, an inflammation of the prostate, can also involve the fibromuscular stroma. Inflammation in the stroma can lead to fibrosis, which can contribute to urinary symptoms and pain.
Impact of Fibromuscular Stroma Changes on Prostate Function and Clinical Outcomes
Alterations within the fibromuscular stroma can have profound effects on prostate function and clinical outcomes. For instance, changes in the stromal composition, such as increased fibrosis, can affect the prostate’s ability to contract and relax, impacting urine flow and contributing to urinary symptoms. The stroma’s role in regulating the prostate’s microenvironment also influences the success of various treatments for prostate disorders.
- BPH: The fibromuscular stroma is a target for several BPH treatments. For example, alpha-blockers, commonly used for BPH, work by relaxing the smooth muscle in the stroma, improving urine flow.
- Prostate Cancer: Understanding the interaction between stromal cells and prostate cancer cells is crucial for developing effective treatments. Targeting stromal cells to suppress tumor growth or prevent metastasis is a promising area of research.
- Prostatitis: Treatments for prostatitis often focus on reducing inflammation and relieving pain. Understanding the role of the fibromuscular stroma in prostatitis could lead to more targeted therapies.
Potential Therapeutic Targets Related to the Fibromuscular Stroma
The fibromuscular stroma presents a rich landscape for potential therapeutic targets in the treatment of prostate disorders.
- Stromal Cell-Derived Factors: Targeting specific factors secreted by stromal cells, such as growth factors or cytokines, could offer new strategies for treating prostate cancer and BPH.
- Stromal Remodeling: Manipulating the stromal microenvironment, such as reducing fibrosis or promoting angiogenesis, could improve prostate function and clinical outcomes.
- Stromal Cell-Based Therapies: Utilizing stromal cells as a therapeutic tool, such as stem cell therapy, is being investigated for its potential in prostate regeneration and treatment of prostate disorders.
Research Directions and Future Perspectives
The fibromuscular stroma (FMS) of the prostate is a complex and dynamic tissue that plays a crucial role in prostate health and disease. Ongoing research is unraveling the intricate interplay between the FMS and various prostate conditions, paving the way for novel diagnostic and therapeutic strategies.
Understanding the Role of FMS in Prostate Cancer, What is the fibromuscular stroma of the prostate
The intricate relationship between the FMS and prostate cancer progression is a major focus of research. Studies are investigating the molecular mechanisms by which the FMS influences tumor growth, invasion, and metastasis. Understanding the specific pathways involved in this interaction could lead to the development of targeted therapies that specifically target the FMS to inhibit cancer progression.
Investigating the Role of FMS in Benign Prostatic Hyperplasia (BPH)
BPH, a common condition characterized by prostate enlargement, is often associated with alterations in the FMS. Researchers are examining the role of the FMS in the development and progression of BPH. This research aims to identify potential therapeutic targets within the FMS that could be manipulated to alleviate symptoms and improve treatment outcomes for BPH.
Exploring the FMS in Prostate Inflammation
Prostatitis, or inflammation of the prostate, can significantly impact prostate health. Researchers are exploring the role of the FMS in the pathogenesis of prostatitis. Understanding the specific contributions of the FMS to inflammation could lead to the development of targeted therapies aimed at reducing inflammation and improving patient outcomes.
Developing Novel Diagnostic Tools
The FMS holds promise as a potential target for novel diagnostic tools. Researchers are exploring the use of biomarkers derived from the FMS to detect prostate cancer at earlier stages, when treatment is most effective. Additionally, the FMS could be utilized for imaging techniques that can accurately identify and characterize prostate lesions.
Developing Targeted Therapies
The FMS presents a unique opportunity for the development of targeted therapies for prostate disorders. Researchers are exploring the potential of using FMS-specific drugs or therapies to inhibit tumor growth, reduce inflammation, or alleviate symptoms of BPH.
The potential applications of this knowledge are vast, ranging from early detection and personalized treatment to the development of novel therapies that specifically target the FMS.
Understanding the intricate structure and function of the fibromuscular stroma is essential for comprehending prostate health and disease. Continued research in this area holds promise for developing novel diagnostic and therapeutic approaches for prostate disorders, improving the lives of millions affected by these conditions.
Question & Answer Hub
What is the significance of the fibromuscular stroma in prostate development?
The fibromuscular stroma plays a crucial role in prostate development, providing structural support and influencing the growth and differentiation of prostate epithelial cells. It contributes to the formation of the gland’s lobules and ducts, which are essential for normal prostate function.
How does the fibromuscular stroma contribute to prostate function?
The fibromuscular stroma plays a vital role in prostate function, particularly in regulating urine flow and sperm transport. Its smooth muscle cells contract and relax, contributing to the control of urine flow through the urethra. Additionally, the stroma provides a supportive framework for the epithelial cells responsible for producing seminal fluid, which nourishes and transports sperm.
What are some potential therapeutic targets related to the fibromuscular stroma for treating prostate disorders?
Research into the fibromuscular stroma has identified potential therapeutic targets for treating prostate disorders. For example, targeting the signaling pathways involved in stromal cell proliferation and differentiation could offer new approaches to managing BPH. Similarly, understanding the role of the stroma in prostate cancer development could lead to novel therapies that inhibit tumor growth and metastasis.






