What is the meaning of central echogenic stroma? This seemingly simple question holds a profound significance in the realm of medical imaging, particularly in the context of prenatal development. Central echogenic stroma, often observed on ultrasound examinations, is a dense, echogenic area located in the center of the fetal brain. Its presence can be a source of both curiosity and concern for expectant parents and medical professionals alike.
Understanding the nature of central echogenic stroma requires a nuanced approach, delving into its anatomical location, developmental processes, and clinical implications. This echogenic structure, a focal point of interest in fetal brain imaging, can provide valuable insights into the health and development of the unborn child.
Central Echogenic Stroma
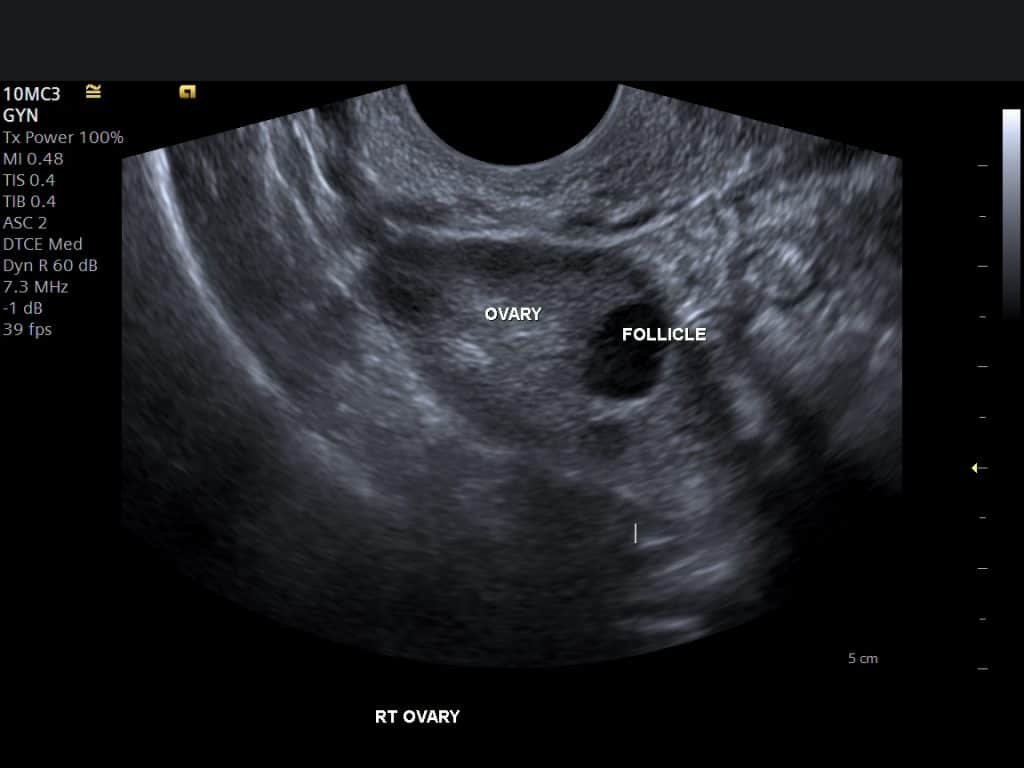
Central echogenic stroma (CES) is a term used in medical imaging, specifically ultrasound, to describe a bright, echo-producing structure located in the center of the ovary.
Definition and Anatomical Location
The central echogenic stroma represents the core of the ovary, composed primarily of connective tissue, blood vessels, and stromal cells. These cells are responsible for producing hormones and supporting the development of follicles, which contain developing eggs. The CES appears bright on ultrasound due to the dense structure of the connective tissue and the presence of blood vessels, which reflect sound waves effectively.
Significance of Central Echogenic Stroma
The presence and appearance of the CES on ultrasound can provide valuable information about ovarian health and function.
- Normal Ovaries: In healthy ovaries, the CES is typically small and well-defined, with a homogeneous appearance.
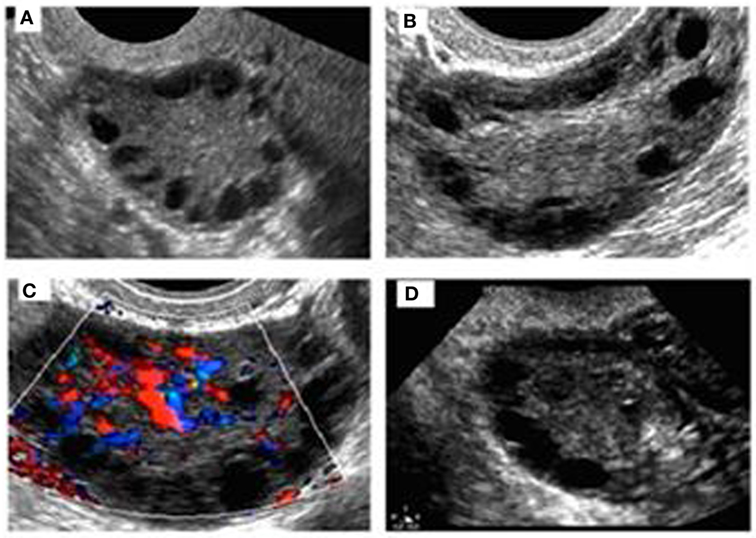
- Polycystic Ovarian Syndrome (PCOS): In PCOS, the CES may be enlarged and more prominent, often accompanied by multiple small follicles around the periphery of the ovary.
- Ovarian Tumors: The presence of a large, irregular, or heterogeneous CES can be a sign of an ovarian tumor. However, it’s important to note that a normal CES doesn’t rule out the possibility of a tumor, and further investigation is often required.
- Ovarian Cysts: The CES may be displaced or distorted by ovarian cysts.
CES in Pregnancy
The CES can also be observed during pregnancy.
- Early Pregnancy: In early pregnancy, the CES may be enlarged and more echogenic due to increased blood flow and hormonal activity.
- Later Pregnancy: In later pregnancy, the CES may be less prominent as the ovary prepares for the delivery of the baby.
Formation and Appearance of Central Echogenic Stroma
The central echogenic stroma (CES) is a bright, echo-rich structure that appears in the fetal brain on ultrasound images. It’s a normal finding in early pregnancy, but its appearance and significance can change throughout gestation. Understanding its formation and how it looks on ultrasound is crucial for accurate fetal assessment.
Formation of Central Echogenic Stroma, What is the meaning of central echogenic stroma
The CES forms during the early stages of brain development. It’s composed of a dense collection of cells and fibers located in the center of the fetal brain. These cells and fibers are responsible for creating the connections between different parts of the brain, laying the foundation for future brain function.
Appearance of Central Echogenic Stroma on Ultrasound Images
On ultrasound, the CES appears as a bright, white, echo-rich structure within the fetal brain. Its size and shape can vary depending on the gestational age. Typically, it’s located in the midline of the brain, between the two hemispheres.
Variations in Appearance of Central Echogenic Stroma
The appearance of the CES can vary depending on factors like gestational age, underlying conditions, and individual fetal development.
- Gestational Age: In the early stages of pregnancy (first trimester), the CES is often more prominent and larger. As the pregnancy progresses, the CES usually becomes smaller and less prominent, eventually disappearing as the brain develops.
- Underlying Conditions: In some cases, the CES may appear larger or more prominent than expected, which can be associated with certain fetal conditions. For example, a larger CES might be seen in fetuses with certain genetic disorders, such as trisomy 21 (Down syndrome).
- Individual Fetal Development: The appearance of the CES can also vary based on individual fetal development. Some fetuses may have a more prominent CES than others, even in the absence of any underlying condition.
Clinical Implications of Central Echogenic Stroma
Central echogenic stroma (CES) is a sonographic finding that can be observed during prenatal ultrasounds. While its presence is often benign, it can be associated with certain medical conditions. Understanding the clinical implications of CES is crucial for proper prenatal care and decision-making.
Medical Conditions Associated with Central Echogenic Stroma
CES is often associated with various medical conditions, some of which may require further investigation and monitoring. The presence of CES can be a marker for potential chromosomal abnormalities, genetic syndromes, or other developmental issues.
- Trisomy 21 (Down syndrome): CES is observed in a significant percentage of fetuses with Down syndrome. This association highlights the importance of further investigations, such as genetic testing, when CES is detected.
- Trisomy 18 (Edwards syndrome): CES is also associated with Edwards syndrome, a rare genetic disorder that can lead to severe health complications.
- Other chromosomal abnormalities: CES can be associated with other chromosomal abnormalities, such as trisomy 13 (Patau syndrome), although less frequently than with Down syndrome or Edwards syndrome.
- Genetic syndromes: Certain genetic syndromes, like Turner syndrome, can also present with CES. These syndromes may involve a range of physical and developmental characteristics.
- Congenital heart defects: In some cases, CES may be associated with congenital heart defects, particularly those affecting the right ventricle.
- Other developmental issues: CES can sometimes be a marker for other developmental issues, such as intrauterine growth restriction (IUGR) or fetal hydrops.
Clinical Relevance of Central Echogenic Stroma
The presence or absence of CES can have significant clinical implications, influencing the course of prenatal care and management.
- Increased risk of chromosomal abnormalities: The presence of CES significantly increases the risk of chromosomal abnormalities, particularly Down syndrome and Edwards syndrome. This necessitates further investigations, such as genetic testing, to confirm or rule out these conditions.
- Monitoring for complications: CES can be a marker for potential complications, such as congenital heart defects or IUGR. Regular ultrasounds and fetal monitoring are crucial to assess fetal growth and development.
- Reassurance and counseling: In many cases, CES is benign and does not indicate any underlying medical conditions. Providing reassurance and counseling to expectant parents is essential, particularly when CES is found to be isolated and not associated with other abnormalities.
Potential Risks and Benefits of Central Echogenic Stroma
While CES can be a marker for potential complications, it’s important to note that its presence does not automatically signify a serious medical condition.
- Potential risks: The main risk associated with CES is the increased risk of chromosomal abnormalities and other developmental issues. Early detection through ultrasound allows for timely interventions and management strategies.
- Potential benefits: CES can be a valuable tool for early detection of potential complications, enabling prompt diagnosis and intervention. This can improve the outcome for both the mother and the fetus.
Differential Diagnosis and Further Investigations
While central echogenic stroma (CES) is often associated with normal fetal development, it’s crucial to consider other potential causes that may necessitate further investigation. This is particularly important when CES is observed alongside other abnormalities or when it persists beyond the expected timeframe.
A comprehensive approach involving a combination of clinical evaluation, ultrasound imaging, and potentially additional investigations is essential to differentiate CES from other conditions and to guide appropriate management.
Differential Diagnosis
The differential diagnosis for CES includes a range of conditions that can present with similar echogenic appearances on ultrasound. It’s important to consider the clinical context, gestational age, and presence of associated abnormalities when evaluating CES.
- Normal Fetal Development: CES is a common finding in the second trimester and often resolves by the third trimester. It’s considered a normal variant in most cases.
- Teratoma: A teratoma is a tumor composed of various tissues, often containing echogenic components. It may appear as a large, complex mass with cystic and solid components, and may be associated with other fetal abnormalities.
- Hematoma: A hematoma within the ovary or other pelvic structures can appear echogenic. It may be associated with pain or other symptoms.
- Fibroids: Uterine fibroids, especially those located in the uterine wall near the fetal pole, can sometimes mimic CES. Fibroids are more common in older women.
- Calcifications: Calcifications within the placenta or fetal tissues can appear echogenic. These can be associated with various conditions, including infections or genetic disorders.
- Other Conditions: Other conditions that can cause echogenic areas include cysts, tumors, and infections. The specific appearance and location of the echogenic area can help narrow down the differential diagnosis.
Recommended Investigations
The choice of investigations will depend on the clinical presentation, gestational age, and ultrasound findings. Here’s a flowchart outlining a potential approach:
| Finding | Investigation |
|---|---|
| CES alone, without other abnormalities | Repeat ultrasound in 2-4 weeks |
| CES with other abnormalities | Detailed fetal anatomy ultrasound, amniocentesis, fetal MRI |
| CES persisting beyond 3rd trimester | Fetal MRI, genetic testing |
| CES with abnormal blood flow | Doppler ultrasound, fetal MRI |
Additional Imaging Modalities and Tests
In certain cases, additional imaging modalities or tests may be necessary to clarify the nature of CES. These include:
- Fetal MRI: Provides more detailed anatomical information and can help differentiate CES from other conditions.
- Amniocentesis: A procedure to obtain amniotic fluid for genetic testing, which can help rule out certain genetic disorders associated with CES.
- Doppler Ultrasound: Used to assess blood flow within the fetal tissues, which can help identify abnormalities associated with CES.
- Genetic Testing: May be recommended if there is a suspicion of a genetic disorder or if other abnormalities are present.
Management and Follow-up: What Is The Meaning Of Central Echogenic Stroma
The management of central echogenic stroma (CES) depends largely on the associated clinical findings and the patient’s individual circumstances. In many cases, CES is an isolated finding and requires no specific intervention. However, in cases where CES is associated with other abnormalities, further investigation and management may be necessary.
Follow-up Examinations and Monitoring
The frequency and nature of follow-up examinations for patients with CES are guided by the associated clinical findings. For instance, if CES is identified in a fetus with other structural abnormalities, more frequent and detailed ultrasound examinations may be recommended.
- For isolated CES, routine prenatal ultrasound examinations are usually sufficient. However, if there are concerns about fetal growth or other potential complications, additional examinations may be recommended.
- In cases of CES associated with other abnormalities, such as chromosomal abnormalities or genetic syndromes, a more tailored follow-up plan may be necessary. This may involve additional ultrasound examinations, fetal echocardiography, and genetic testing.
- After birth, infants with CES should be monitored for any signs of developmental delays or other health problems. Regular check-ups with a pediatrician are essential.
Role of Genetic Counseling
Genetic counseling can be beneficial for families with CES, particularly when it is associated with other abnormalities. A genetic counselor can provide information about the potential causes of CES, the risks of recurrence, and the available testing options.
- Genetic counseling can help families understand the implications of CES and make informed decisions about future pregnancies.
- In cases of CES associated with chromosomal abnormalities or genetic syndromes, genetic counseling can help families navigate the complex medical and emotional aspects of these conditions.
Research and Future Directions
While significant progress has been made in understanding central echogenic stroma (CES), several research gaps and areas for future investigation remain. These areas hold the potential to enhance our understanding of CES, improve its diagnostic accuracy, and ultimately lead to more effective management strategies.
Current Research Gaps and Areas for Future Investigations
- The exact mechanisms underlying the formation of CES in different clinical scenarios are not fully understood. Further research is needed to elucidate the role of various factors, including genetic predisposition, maternal health, and environmental influences, in CES development.
- The prognostic significance of CES in various clinical settings, particularly in relation to fetal outcomes, requires further investigation. Longitudinal studies are needed to determine the correlation between CES presence, characteristics, and subsequent fetal development, including the risk of adverse outcomes.
- The optimal management strategies for CES, particularly in cases where it is associated with fetal anomalies, need to be refined. Clinical trials are necessary to evaluate the efficacy of different approaches, including expectant management, invasive procedures, and genetic counseling, in different clinical contexts.
Potential Research Questions and Hypotheses
The following research questions and hypotheses could guide future investigations into the clinical significance and management of CES:
- Does the size, location, and echogenicity of CES correlate with specific fetal anomalies or developmental issues?
- Can specific biomarkers or genetic markers be identified to predict the risk of adverse outcomes in fetuses with CES?
- Do different management strategies, such as expectant management versus invasive procedures, affect the long-term outcomes of fetuses with CES?
Impact of Emerging Technologies on Understanding and Management
Advancements in medical imaging technologies, such as 3D/4D ultrasound, fetal MRI, and advanced genetic testing, hold significant promise for improving the understanding and management of CES.
- 3D/4D ultrasound can provide more detailed anatomical information about the fetus and CES, allowing for more accurate assessment of fetal development and potential complications.
- Fetal MRI offers superior soft tissue resolution compared to ultrasound, enabling the detection of subtle fetal anomalies associated with CES that may not be visible on ultrasound.
- Advanced genetic testing, such as whole-exome sequencing, can help identify genetic mutations associated with CES and provide insights into the underlying pathogenesis.
Central echogenic stroma, while often a cause for concern, is not always a harbinger of adverse outcomes. The interpretation of its presence requires careful consideration of the gestational age, associated clinical findings, and the expertise of medical professionals. As our understanding of fetal development and imaging technologies continue to advance, we are better equipped to manage cases involving central echogenic stroma, ensuring the best possible care for both mother and child.
Question & Answer Hub
Is central echogenic stroma always a sign of a problem?
No, central echogenic stroma is not always indicative of a problem. In many cases, it is a benign finding that resolves on its own. However, it is important to be evaluated by a medical professional to rule out any underlying conditions.
What are the potential causes of central echogenic stroma?
The exact cause of central echogenic stroma is not always known. It can be associated with various factors, including genetic predisposition, infections, or developmental abnormalities.
What are the risks associated with central echogenic stroma?
The risks associated with central echogenic stroma depend on the underlying cause and other clinical findings. In some cases, it may be associated with an increased risk of developmental delays or neurological disorders.
What kind of follow-up is recommended after a diagnosis of central echogenic stroma?
The recommended follow-up depends on the individual case and the findings. It may include additional ultrasounds, fetal MRI, or genetic testing.





