What is cervical stroma? It’s a hidden world within the cervix, a complex network of connective tissue, blood vessels, and nerves that plays a vital role in the health and function of this crucial organ. Imagine it as the scaffolding that provides structure and support for the cervical epithelium, the protective layer that lines the cervix. But the cervical stroma does much more than just hold things together.
It’s a dynamic player in the intricate processes of cervical development, maturation, and even repair.
Think of the cervical stroma as a conductor, orchestrating the delicate balance of the cervix. It influences the production of mucus, which acts as a gatekeeper, controlling the flow of substances into the uterus. It also plays a crucial role in cervical dilation, allowing for the passage of a baby during childbirth.
Definition and Structure of Cervical Stroma
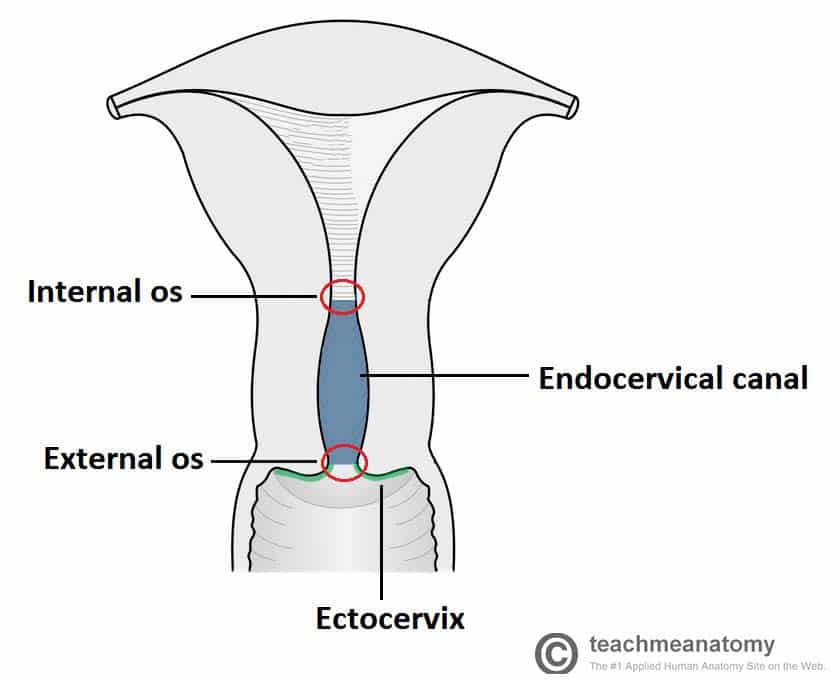
The cervical stroma, a crucial component of the cervix, is a dense, supportive connective tissue that lies beneath the epithelial lining. It plays a vital role in maintaining the structural integrity of the cervix and providing a framework for the passage of the fetus during childbirth.
Components of Cervical Stroma
The cervical stroma is composed of various elements that work together to provide support and functionality. These include:
- Connective Tissue: The primary component of the stroma is connective tissue, primarily composed of collagen fibers. These fibers are arranged in a dense, interwoven network, providing strength and elasticity to the cervix. This arrangement allows the cervix to stretch and dilate during labor, while maintaining its structural integrity.
- Blood Vessels: A rich network of blood vessels permeates the cervical stroma, supplying oxygen and nutrients to the epithelial lining and supporting cells. These vessels also play a role in removing waste products and regulating cervical blood flow.
- Nerves: Sensory nerves are present within the stroma, providing feedback to the central nervous system regarding cervical tension and dilation. This feedback is essential for coordinating the physiological changes that occur during labor and delivery.
Role of Cervical Stroma in Supporting the Cervical Epithelium
The cervical stroma provides a crucial foundation for the cervical epithelium, the protective lining of the cervix. The dense network of collagen fibers within the stroma acts as a scaffold, providing structural support and anchoring the epithelium. This support is essential for maintaining the integrity of the epithelial barrier, preventing infections and maintaining normal cervical function.
Functions of Cervical Stroma
The cervical stroma plays a crucial role in the development, maturation, and function of the cervix. It provides structural support, participates in tissue regeneration, and influences various physiological processes within the cervix.
Role in Cervical Development and Maturation
The cervical stroma is essential for the proper development and maturation of the cervix. During fetal development, the stroma undergoes significant changes, contributing to the formation of the cervical canal and the differentiation of cervical cells.
- The stroma provides a framework for the developing cervix, guiding the growth and organization of the cervical tissues.
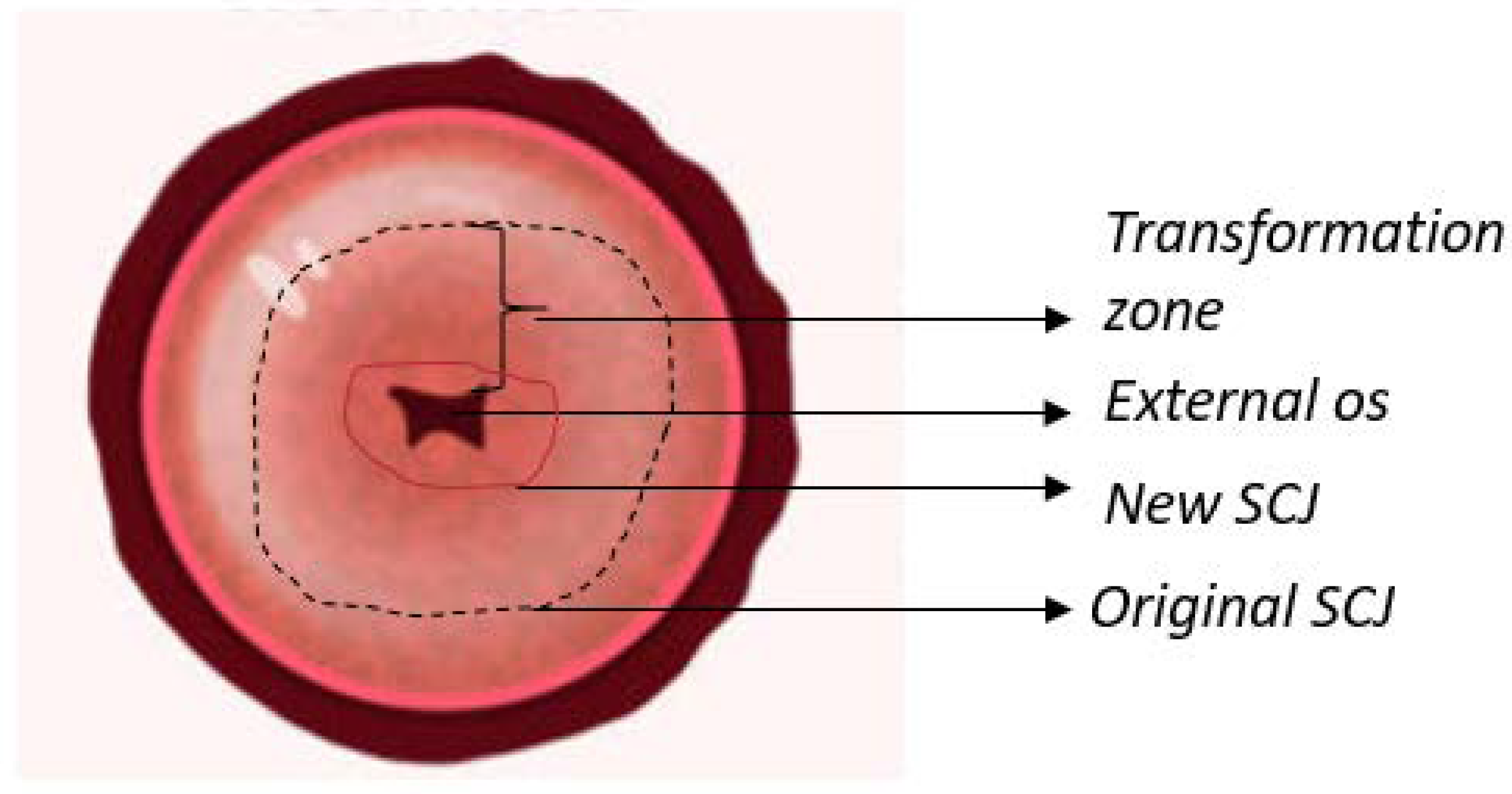
- It also secretes factors that promote the differentiation of cervical epithelial cells, leading to the formation of the specialized layers of the cervix, including the squamous epithelium and the endocervical epithelium.
As the cervix matures, the stroma continues to play a role in maintaining its structure and function.
Contribution to Cervical Tissue Regeneration and Repair
The cervical stroma is actively involved in the regeneration and repair of cervical tissues following injury or damage.
- It contains a population of stromal cells that have the potential to differentiate into various cell types, including fibroblasts, myofibroblasts, and endothelial cells.
- These cells contribute to the formation of new connective tissue, blood vessels, and other structures necessary for tissue repair.
The stromal cells also produce growth factors and cytokines that stimulate the proliferation and differentiation of other cell types, further promoting tissue regeneration.
Regulation of Cervical Function
The cervical stroma plays a significant role in regulating various cervical functions, including mucus production and cervical dilation.
- The stroma provides a supportive environment for the cervical glands, which are responsible for producing mucus.
- It secretes factors that influence the activity of these glands, regulating the amount and composition of cervical mucus.
- During pregnancy, the stroma undergoes hormonal changes that contribute to cervical softening and dilation, facilitating childbirth.
The cervical stroma also contributes to the regulation of cervical blood flow, which is essential for maintaining the health and function of the cervix.
Cervical Stroma in Health and Disease
The cervical stroma, a dynamic and responsive tissue, undergoes significant changes throughout a woman’s life, particularly during the menstrual cycle and pregnancy. It also plays a crucial role in the development and progression of cervical cancer, making it a key target for therapeutic interventions.
Changes in Cervical Stroma During the Menstrual Cycle and Pregnancy
The cervical stroma exhibits cyclical changes in response to hormonal fluctuations during the menstrual cycle. During the follicular phase, estrogen dominance stimulates the proliferation of stromal cells, leading to an increase in cervical mucus production. This mucus is thin and watery, facilitating sperm transport. As the cycle progresses, progesterone levels rise during the luteal phase, causing the stroma to become more compact and the mucus to thicken, creating a barrier that impedes sperm entry.During pregnancy, the cervical stroma undergoes profound changes to accommodate the growing fetus and facilitate labor.
Estrogen and progesterone levels remain elevated, leading to further stromal cell proliferation and increased vascularization. The cervix softens and dilates, preparing for the passage of the baby during labor.
Role of Cervical Stroma in the Pathogenesis of Cervical Cancer
The cervical stroma plays a complex role in the development and progression of cervical cancer. While it normally provides structural support and regulates cervical function, it can become compromised in the presence of cancer cells. Cancer cells can interact with the stroma in several ways:
- Stromal Remodeling: Cancer cells can induce changes in the stromal microenvironment, leading to increased vascularization, angiogenesis, and inflammation. These changes provide nutrients and growth factors to the tumor, promoting its growth and spread.
- Immune Suppression: The stroma can be infiltrated by immune cells, but cancer cells can manipulate these cells to suppress the immune response, allowing the tumor to evade destruction.
- Metastasis: The stroma can serve as a conduit for cancer cells to spread to distant sites. Cancer cells can invade the stroma and migrate through it, ultimately reaching lymph nodes and other organs.
Targeting Cervical Stroma for Therapeutic Interventions
The intimate relationship between cervical stroma and cancer cells has opened up new avenues for therapeutic interventions. Several strategies are being investigated to target the stroma and inhibit tumor growth:
- Anti-angiogenic Therapies: These therapies aim to block the formation of new blood vessels that supply the tumor with nutrients and oxygen. This can be achieved by targeting specific growth factors or signaling pathways involved in angiogenesis.
- Immune Checkpoint Inhibitors: These drugs activate the immune system to recognize and attack cancer cells. They work by blocking inhibitory signals that prevent immune cells from killing tumor cells. For example, the drug pembrolizumab targets the PD-1 pathway, which is often upregulated in cervical cancer cells, allowing them to evade immune destruction.
- Stromal Targeting Therapies: This approach focuses on directly targeting the stroma to modify its interactions with cancer cells. For instance, drugs that disrupt the extracellular matrix, the scaffold that supports the stroma, can inhibit tumor invasion and metastasis. Other therapies aim to re-educate stromal cells to suppress tumor growth or enhance the anti-tumor immune response.
Clinical Significance of Cervical Stroma: What Is Cervical Stroma
The cervical stroma plays a crucial role in the development and progression of cervical cancer, making it a vital target for diagnosis, staging, and monitoring. Its unique composition and interaction with other cervical tissues provide valuable insights into the disease’s progression and response to treatment.
Cervical Stromal Biopsies in Diagnosis and Staging of Cervical Cancer
Cervical stromal biopsies are essential for the accurate diagnosis and staging of cervical cancer. They involve obtaining a small sample of cervical stroma tissue for microscopic examination. This procedure helps pathologists identify the presence of cancerous cells and determine the extent of tumor invasion.
- Diagnosis: Stromal biopsies can differentiate between benign and malignant lesions, confirming the presence of cervical cancer. They also help classify the type of cancer, such as squamous cell carcinoma or adenocarcinoma, which guides treatment decisions.
- Staging: The depth of stromal invasion by cancerous cells is a crucial factor in determining the cancer’s stage, which influences treatment options and prognosis. Stages are typically classified as follows:
- Stage I: Cancer confined to the cervix.
- Stage II: Cancer has spread beyond the cervix but not to the pelvic wall.
- Stage III: Cancer has spread to the pelvic wall or has involved the lower third of the vagina.
- Stage IV: Cancer has spread to distant organs.
Role of Cervical Stroma in Cervical Cancer Screening and Early Detection
Cervical stromal changes associated with precancerous lesions and early-stage cervical cancer can be detected through various screening methods, facilitating early detection and intervention.
- Pap Smear: This test involves collecting cells from the cervix and examining them for abnormalities. While primarily focusing on cervical epithelial cells, it can also reveal changes in the stromal tissue, such as increased cellularity or inflammation, which can indicate precancerous conditions.
- Human Papillomavirus (HPV) Testing: HPV infection is a major risk factor for cervical cancer. HPV testing identifies the presence of high-risk HPV strains, which can trigger abnormal cellular changes in the cervix and potentially lead to cancer. While primarily targeting epithelial cells, HPV testing indirectly assesses the stromal environment as HPV infection can induce stromal inflammation and cellular alterations.
- Colposcopy: This procedure uses a magnifying device to visualize the cervix and obtain biopsies from suspicious areas. Colposcopy allows for a more detailed examination of the cervical stroma, enabling the detection of early-stage cancer and precancerous lesions.
Cervical Stroma as a Source of Biomarkers for Cervical Cancer Diagnosis and Prognosis
The cervical stroma harbors a wealth of molecular information that can serve as potential biomarkers for cervical cancer diagnosis and prognosis. These biomarkers can provide insights into the disease’s aggressiveness, predict treatment response, and monitor disease recurrence.
- Microenvironment Analysis: Analyzing the composition and function of stromal cells, such as fibroblasts, immune cells, and blood vessels, can reveal critical information about the tumor’s microenvironment. For example, increased stromal angiogenesis (blood vessel formation) can indicate tumor growth and spread.
- Gene Expression Profiling: Studying gene expression patterns in stromal cells can identify specific molecular signatures associated with cervical cancer development and progression. These signatures can be used to classify tumors, predict patient outcomes, and guide treatment strategies.
- Proteomic Analysis: Examining the protein profile of stromal cells can reveal biomarkers associated with tumor growth, invasion, and metastasis. These biomarkers can be used to monitor disease progression and response to treatment.
Research and Future Directions
The cervical stroma, a dynamic and multifaceted tissue, has garnered increasing research interest due to its crucial role in cervical health and disease. Recent advancements in molecular and cellular biology have shed light on the intricate mechanisms governing cervical stroma function, opening new avenues for therapeutic interventions and regenerative medicine applications.
Advancements in Understanding Cervical Stroma Function
Our understanding of cervical stroma function has been significantly enhanced by recent research, particularly in the areas of molecular signaling pathways, cellular interactions, and the role of the extracellular matrix (ECM).
- Signaling Pathways: Studies have revealed the involvement of various signaling pathways, such as the Wnt, TGF-β, and Hedgehog pathways, in regulating cervical stroma development, ECM remodeling, and immune cell recruitment. Understanding these pathways provides valuable insights into the mechanisms underlying cervical stromal dysfunction in disease states.
- Cellular Interactions: The cervical stroma is a complex microenvironment composed of various cell types, including fibroblasts, immune cells, and epithelial cells. Recent research has elucidated the intricate interactions between these cells, highlighting the importance of cell-cell communication in maintaining cervical stromal homeostasis.
- Extracellular Matrix: The ECM, a complex network of proteins and polysaccharides, plays a vital role in providing structural support, regulating cell behavior, and mediating signaling pathways within the cervical stroma. Recent studies have focused on the composition and dynamics of the ECM in cervical health and disease, revealing its potential as a therapeutic target.
Therapeutic Strategies Targeting Cervical Stroma, What is cervical stroma
The emerging understanding of cervical stroma function has paved the way for the development of novel therapeutic strategies targeting this tissue.
- Targeting Signaling Pathways: By modulating specific signaling pathways, researchers aim to restore cervical stromal function in disease states. For example, targeting the Wnt pathway has shown promise in treating cervical cancer, while inhibiting the TGF-β pathway may be beneficial in managing cervical fibrosis.
- Modulating ECM Composition: Manipulating the ECM composition and organization has emerged as a promising therapeutic approach. Strategies include using ECM-derived biomaterials to promote tissue regeneration or targeting specific ECM components to modulate cell behavior.
- Immune Cell Modulation: The cervical stroma plays a crucial role in regulating immune responses. Research efforts are focused on developing therapies that modulate immune cell activity within the cervical stroma to enhance immune surveillance and target disease-associated cells.
Bioengineered Cervical Stroma for Regenerative Medicine
The potential of bioengineered cervical stroma for regenerative medicine applications is gaining significant attention.
- Tissue Engineering: Researchers are exploring the use of bioengineered cervical stroma for reconstructing damaged cervical tissues, such as after surgery or injury. This approach involves using biomaterials, growth factors, and cells to create functional cervical stromal tissues in vitro.
- Drug Delivery: The cervical stroma can serve as a platform for targeted drug delivery. Bioengineered cervical stromal tissues can be loaded with therapeutic agents and implanted at the desired site, enabling localized and sustained drug release.
- Disease Modeling: Bioengineered cervical stroma can be used to develop in vitro models of cervical diseases, facilitating drug screening and research on disease mechanisms.
From its role in cervical development and function to its potential as a target for therapeutic interventions, the cervical stroma is a vital component of the female reproductive system. Understanding this hidden world is key to unlocking new insights into cervical health and disease, paving the way for more effective diagnostic tools and treatments.
Query Resolution
What is the difference between cervical stroma and cervical epithelium?
The cervical epithelium is the layer of cells that lines the surface of the cervix, while the cervical stroma is the underlying connective tissue that provides support and structure.
Can cervical stroma be affected by hormonal changes?
Yes, cervical stroma is influenced by hormonal changes throughout the menstrual cycle and pregnancy. These fluctuations affect its composition and function.
How does cervical stroma relate to cervical cancer?
Cervical stroma plays a role in the development and progression of cervical cancer. Changes in the stroma can contribute to the growth and spread of cancer cells.






