What is echogenic stroma? This intriguing term, often encountered in the realm of medical imaging, refers to a bright, white appearance on ultrasound scans, indicating dense or thickened tissue. Echogenic stroma can arise in various organs and tissues, potentially signifying a range of conditions, from benign to more serious. Understanding the nature and significance of echogenic stroma is crucial for accurate diagnosis and appropriate treatment planning.
The appearance of echogenic stroma on ultrasound is characterized by its high echogenicity, reflecting sound waves strongly back to the transducer. This bright, white appearance contrasts with the darker, more fluid-filled areas often seen in healthy tissues. The specific pattern and location of echogenic stroma can provide valuable clues to its underlying cause. For instance, echogenic stroma in the ovaries may suggest a cyst or a fibroid, while in the breast, it could indicate a tumor or inflammation.
Further evaluation, including additional imaging and biopsies, may be necessary to determine the precise nature of echogenic stroma and guide treatment decisions.
What is Echogenic Stroma?

Echogenic stroma, a term frequently encountered in medical imaging, particularly ultrasound, refers to areas within an organ or tissue that appear brighter than the surrounding tissue. This brightness, or echogenicity, is caused by the reflection of sound waves from the dense structures within the stroma. Think of it like shining a flashlight into a dense forest; the light bounces back more intensely from the dense foliage than from open spaces.
Appearance of Echogenic Stroma on Ultrasound Scans
Echogenic stroma is typically visualized as a white or bright area on an ultrasound image. The intensity of the echogenicity can vary, with some areas appearing as solid white, while others may have a more speckled or granular appearance. The specific appearance of echogenic stroma can provide clues about the underlying tissue composition and potential abnormalities.
Examples of Different Echogenic Stroma Patterns and their Potential Significance
The appearance of echogenic stroma can vary significantly, depending on the tissue and the underlying cause. Here are some examples:
Echogenic Stroma in the Ovaries
In the ovaries, echogenic stroma can be seen in several different patterns. For example, a “solid” echogenic stroma might indicate a benign ovarian cyst or a fibroma, while a “speckled” echogenic stroma might be associated with a more complex ovarian tumor.
It’s important to note that echogenic stroma alone is not a definitive diagnostic tool. Further evaluation with other imaging modalities or even biopsy may be necessary to confirm the diagnosis.
Echogenic Stroma in the Prostate
In the prostate, echogenic stroma can be a sign of benign prostatic hyperplasia (BPH), a common condition that causes an enlarged prostate. However, it can also be associated with prostate cancer, particularly in men with a family history of the disease.
Echogenic stroma in the prostate is often associated with increased prostate-specific antigen (PSA) levels, a blood test commonly used to screen for prostate cancer.
Echogenic Stroma in the Breast
In the breast, echogenic stroma can be a sign of fibrocystic changes, a common benign condition. However, it can also be associated with breast cancer, particularly in women with a family history of the disease.
Echogenic stroma in the breast is often associated with dense breast tissue, which can make it more difficult to detect breast cancer on mammograms.
Causes of Echogenic Stroma
Echogenic stroma, the bright white areas on an ultrasound, can be caused by a variety of factors. It’s like a spotlight shining on the ovaries, making them appear brighter than usual. While not always a cause for alarm, understanding the potential causes can help guide your doctor in determining the best course of action.
Causes of Echogenic Stroma
Understanding the mechanisms behind echogenic stroma formation is crucial for accurate diagnosis and treatment. Here’s a breakdown of the common causes:
- Fibroids: These benign tumors are like little knots within the uterine wall. They can be dense and filled with collagen, reflecting sound waves strongly and appearing bright on ultrasound. Fibroids are a common cause of echogenic stroma, especially in women of reproductive age.
- Polycystic Ovarian Syndrome (PCOS): In PCOS, the ovaries often develop numerous cysts, which can contribute to echogenic stroma. The cysts themselves are fluid-filled sacs, but the surrounding ovarian tissue can become denser and more echogenic.
- Endometriosis: This condition involves the growth of uterine lining tissue outside the uterus. When endometriosis implants on the ovaries, it can cause scarring and inflammation, leading to echogenic stroma.
- Ovarian Cysts: While most ovarian cysts are benign and resolve on their own, some can become complex and contain solid components. These solid areas can appear echogenic on ultrasound.
- Aging: As women age, their ovaries naturally undergo changes. The ovarian tissue can become more dense and echogenic, reflecting sound waves more strongly.
- Inflammation: Inflammation within the ovaries can also contribute to echogenic stroma. The inflammation can cause the ovarian tissue to become thicker and denser, leading to a brighter appearance on ultrasound.
Common Causes of Echogenic Stroma
Here’s a table summarizing the common causes of echogenic stroma, their associated symptoms, and potential treatments:
| Cause | Symptoms | Treatment |
|---|---|---|
| Fibroids | Heavy menstrual bleeding, pelvic pain, pain during intercourse | Hormonal therapy, surgery (myomectomy or hysterectomy) |
| Polycystic Ovarian Syndrome (PCOS) | Irregular periods, acne, excess hair growth, weight gain, infertility | Lifestyle changes (weight loss, exercise), hormonal therapy, fertility treatments |
| Endometriosis | Painful periods, pelvic pain, pain during intercourse, infertility | Hormonal therapy, surgery, pain management |
| Ovarian Cysts | Pelvic pain, bloating, irregular periods | Observation, hormonal therapy, surgery (cystectomy) |
| Aging | No specific symptoms | None required, regular monitoring |
| Inflammation | Pelvic pain, fever, vaginal discharge | Antibiotics, pain management |
Clinical Significance of Echogenic Stroma
Echogenic stroma, while often a benign finding, can have significant clinical implications depending on the organ or tissue involved. Its presence can be a sign of various underlying conditions, ranging from normal variations to more serious pathologies. Understanding the context and associated findings is crucial for accurate diagnosis and appropriate management.
Echogenic Stroma in Different Organs and Tissues
The significance of echogenic stroma varies depending on the specific organ or tissue where it is observed. Here’s a breakdown of potential implications in different contexts:
- Ovaries: In the ovaries, echogenic stroma can be a normal finding, especially in premenopausal women. However, it can also be associated with conditions like polycystic ovary syndrome (PCOS) or ovarian tumors. Increased echogenicity in the ovarian stroma can indicate an increased number of stromal cells, which may be associated with hormonal imbalances or other conditions.
- Uterus: In the uterus, echogenic stroma can be a sign of fibroids, polyps, or endometrial thickening. These findings may require further investigation to rule out any underlying pathology.
- Breast: In the breast, echogenic stroma can be associated with benign conditions like fibrocystic changes or fibroadenomas. However, it can also be a sign of more serious conditions like breast cancer, especially if accompanied by other suspicious features.
- Prostate: In the prostate, echogenic stroma can be a sign of benign prostatic hyperplasia (BPH), prostatitis, or prostate cancer. The presence of echogenic stroma in the prostate should be carefully evaluated along with other clinical and imaging findings.
- Kidneys: In the kidneys, echogenic stroma can be a sign of chronic kidney disease, glomerulonephritis, or renal scarring. However, it can also be a normal finding in some individuals.
- Liver: In the liver, echogenic stroma can be a sign of fatty liver disease, cirrhosis, or hepatitis. However, it can also be a normal finding in some individuals.
Comparison and Contrast of Echogenic Stroma Significance
Echogenic stroma can be a valuable indicator in different medical contexts, but its significance varies depending on the associated findings and the patient’s overall clinical presentation. Here’s a comparison of its significance in different scenarios:
- Benign vs. Malignant: In many cases, echogenic stroma is associated with benign conditions. However, it can also be a sign of malignancy, especially when accompanied by other suspicious features. For example, echogenic stroma in the breast, when associated with a mass or other abnormal findings, may raise suspicion for breast cancer.
- Normal Variation vs. Pathology: Echogenic stroma can be a normal finding in some organs, such as the ovaries in premenopausal women. However, in other cases, it may indicate an underlying pathology. For example, echogenic stroma in the prostate can be a sign of BPH or prostatitis.
- Acute vs. Chronic: Echogenic stroma can be a sign of both acute and chronic conditions. For example, echogenic stroma in the kidneys can be associated with acute glomerulonephritis or chronic kidney disease.
Diagnostic and Treatment Pathways
The diagnostic and treatment pathways associated with echogenic stroma findings depend on the specific organ or tissue involved, the patient’s clinical presentation, and other associated findings. Here’s a simplified flowchart illustrating a potential diagnostic and treatment pathway:
Echogenic stroma detected on imaging –> Clinical evaluation and history taking –> Further investigations (e.g., biopsies, blood tests) –> Diagnosis –> Treatment (if necessary)
Differential Diagnosis
Echogenic stroma is a common finding on ultrasound, but it’s important to remember that it’s not the only possible explanation for a bright, dense appearance on the scan. Several other conditions can mimic echogenic stroma, and it’s crucial to distinguish between them to ensure accurate diagnosis and appropriate management.The differential diagnosis of echogenic stroma is essential because the underlying cause dictates the treatment approach.
For example, a benign fibroid with echogenic stroma might require no intervention, while a malignant tumor with similar ultrasound features might require immediate biopsy and further evaluation.
Comparison of Ultrasound Features
This table highlights the key features that help differentiate echogenic stroma from other ultrasound abnormalities:
| Feature | Echogenic Stroma | Fibroids | Endometrial Polyp | Ovarian Cyst | Malignancy |
|---|---|---|---|---|---|
| Location | Uterus, typically in the myometrium | Uterus, typically in the myometrium | Endometrial cavity | Ovary | Variable, can be in the uterus, ovaries, or other pelvic organs |
| Shape | Diffuse or focal, often with a heterogeneous appearance | Well-defined, round or oval, often with a smooth border | Pedunculated or sessile, often with a smooth or irregular border | Round or oval, often with a smooth or irregular border | Variable, can be irregular, infiltrative, or nodular |
| Echogenicity | Bright, dense, often with a “salt and pepper” appearance | Bright, dense, often with a homogeneous appearance | Bright, dense, often with a homogeneous appearance | Variable, can be anechoic, hypoechoic, or hyperechoic | Variable, can be hypoechoic, hyperechoic, or complex |
| Blood Flow | Minimal or absent | Minimal or absent | Minimal or absent | Variable, can be absent, low, or high | Variable, can be absent, low, or high |
| Other Features | May be associated with uterine fibroids or other benign conditions | Often associated with heavy menstrual bleeding, pelvic pain, or infertility | Often associated with abnormal uterine bleeding | Often associated with pelvic pain, bloating, or irregular periods | May be associated with abnormal bleeding, pain, or rapid growth |
Remember, the final diagnosis is always based on a combination of clinical history, physical examination, and imaging findings. If you’re concerned about echogenic stroma or other ultrasound findings, it’s important to discuss your concerns with your healthcare provider.
Further Evaluation
Sometimes, even after a thorough ultrasound, the mystery of echogenic stroma remains. It’s like trying to solve a puzzle with missing pieces! In these cases, further evaluation is necessary to get a clearer picture of what’s going on. Think of it like this: You’ve got a blurry photo of a landscape, and you need a better lens to see the details.
Additional imaging and tests can provide that “better lens” to help us understand the echogenic stroma.
Additional Imaging
When the ultrasound isn’t enough to solve the puzzle, additional imaging techniques can provide more detailed information. Here are some examples:
- Magnetic Resonance Imaging (MRI): MRI uses strong magnetic fields and radio waves to create detailed images of organs and tissues. It’s like having a super-powered microscope for your body! MRI can help distinguish between different types of tissue, including benign and malignant growths.
- Computed Tomography (CT) Scan: CT scans use X-rays to create cross-sectional images of the body. Think of it as taking multiple snapshots from different angles to create a 3D image. CT scans can be helpful in identifying the size and location of echogenic stroma, as well as any surrounding structures.
Biopsy, What is echogenic stroma
If additional imaging still leaves some questions unanswered, a biopsy may be recommended. A biopsy involves taking a small sample of tissue for examination under a microscope. It’s like taking a tiny piece of the puzzle to see what it looks like up close.
- Procedure: A biopsy can be performed using different methods, depending on the location of the echogenic stroma. For example, a needle biopsy may be used to sample tissue from the uterus or ovaries, while a surgical biopsy may be necessary for larger or deeper lesions.
- Interpretation: A pathologist will examine the biopsy sample under a microscope to determine the type of tissue present. They’ll look for signs of inflammation, infection, or cancer. This information is crucial for making a diagnosis and guiding treatment.
Management and Treatment

The management and treatment of conditions associated with echogenic stroma depend on the underlying cause and the severity of the symptoms. It’s important to remember that echogenic stroma is not a disease itself, but rather a finding on ultrasound that can be associated with various conditions.
Treatment Options
Treatment options for conditions associated with echogenic stroma vary widely and depend on the specific diagnosis. Here are some common approaches:
Observation
In many cases, especially when the echogenic stroma is mild and not associated with other abnormalities, the best course of action may be to simply observe the situation. Regular ultrasounds can help monitor any changes over time.
Medication
For conditions that are caused by hormonal imbalances or other medical conditions, medication may be prescribed to address the underlying cause. For example, if echogenic stroma is associated with polycystic ovary syndrome (PCOS), medication like metformin or clomiphene citrate may be prescribed.
Surgery
Surgery is rarely necessary for conditions associated with echogenic stroma. However, in some cases, such as when the echogenic stroma is associated with a large fibroid or ovarian cyst, surgery may be required to remove the affected tissue.
Assisted Reproductive Technologies (ART)
For women with infertility associated with echogenic stroma, ART techniques like in vitro fertilization (IVF) may be considered. IVF involves fertilizing eggs outside the body and then transferring the embryos into the uterus.
Risks and Benefits of Treatment Approaches
The following table Artikels the potential risks and benefits of different treatment approaches for conditions associated with echogenic stroma:| Treatment Approach | Risks | Benefits ||—|—|—|| Observation | No immediate risks, but may delay diagnosis or treatment of underlying conditions | Safe, cost-effective, and allows for monitoring of changes over time || Medication | Side effects of medication, potential for drug interactions | Can effectively address underlying medical conditions || Surgery | Complications of surgery, risk of infection, potential for scarring | Can effectively remove affected tissue and relieve symptoms || ART | High cost, potential for multiple cycles, risk of multiple pregnancies | Can increase chances of pregnancy in women with infertility |It’s important to discuss the risks and benefits of all treatment options with your doctor to determine the best course of action for your individual situation.
Prognosis and Follow-up: What Is Echogenic Stroma
The prognosis for patients with echogenic stroma varies depending on the underlying cause and the specific clinical presentation. In many cases, echogenic stroma is an isolated finding with no significant clinical implications. However, it can also be associated with certain conditions that may require further evaluation and management.
Potential Complications and Sequelae
Echogenic stroma, while often benign, can sometimes be associated with complications or sequelae. These can include:
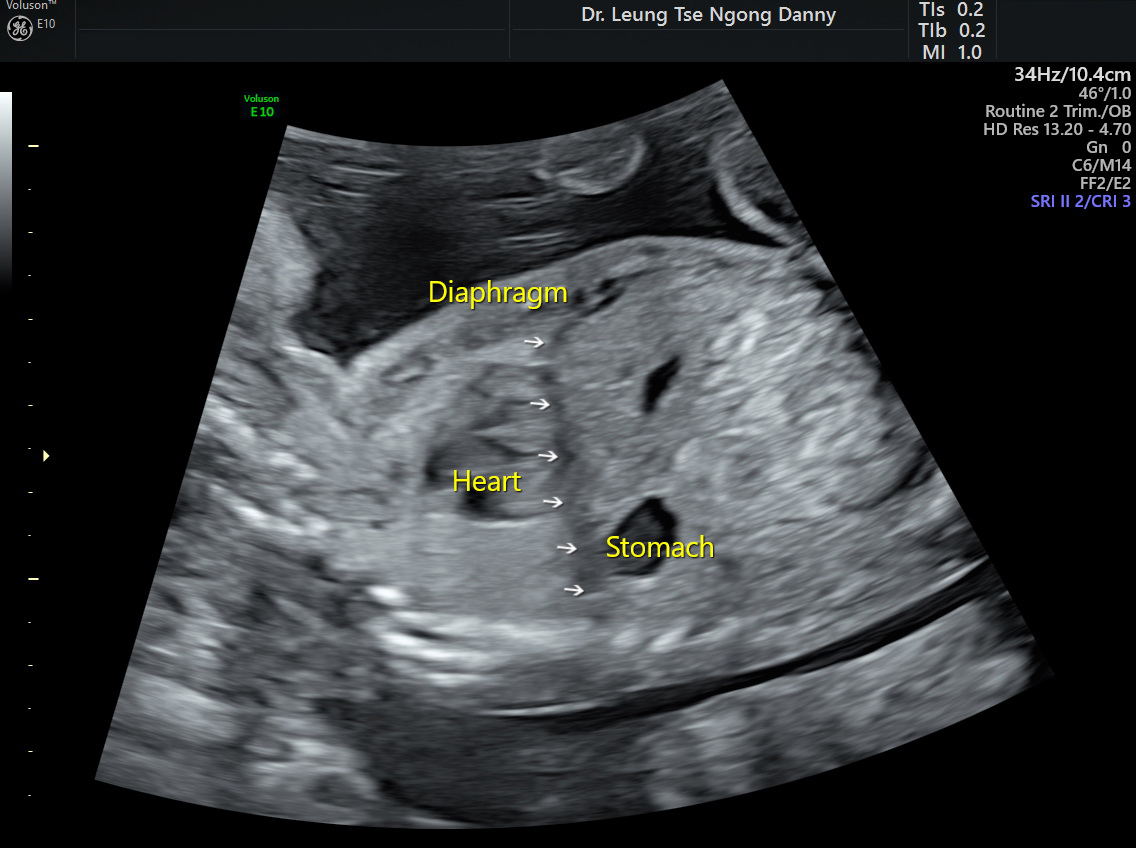
- Chromosomal abnormalities: Echogenic stroma is sometimes associated with chromosomal abnormalities, such as trisomy 21 (Down syndrome). In these cases, the echogenic stroma may be a marker for other developmental abnormalities.
- Congenital heart defects: Echogenic stroma has been linked to an increased risk of congenital heart defects, particularly in cases of trisomy 21. However, the association is not always present, and the presence of echogenic stroma alone does not guarantee the presence of a heart defect.
- Other developmental abnormalities: Echogenic stroma can be associated with other developmental abnormalities, such as renal agenesis (absence of one or both kidneys), diaphragmatic hernia, and neural tube defects. These conditions may require specific medical interventions and long-term management.
Follow-up Care and Monitoring Strategies
Patients with echogenic stroma often require close follow-up care and monitoring to assess for potential complications and to ensure appropriate management. The frequency and type of follow-up will depend on the specific clinical presentation and the presence of any associated conditions.
- Ultrasound scans: Regular ultrasound scans are typically recommended to monitor the size and appearance of the echogenic stroma. These scans can help to assess for any changes in the structure or size of the stroma, which may indicate the presence of a developing complication.
- Genetic testing: In some cases, genetic testing may be recommended to assess for chromosomal abnormalities or other genetic conditions that may be associated with echogenic stroma. This can help to provide a more accurate prognosis and to guide management strategies.
- Cardiac evaluation: If there is a suspicion of a congenital heart defect, a cardiac evaluation may be performed. This can involve an echocardiogram (ultrasound of the heart) or other diagnostic tests to assess the structure and function of the heart.
- Other specialists: Depending on the underlying cause and the specific clinical presentation, patients with echogenic stroma may need to be referred to other specialists, such as a geneticist, cardiologist, or nephrologist. These specialists can provide specialized care and management for any associated conditions.
Echogenic stroma, a visual clue on ultrasound scans, serves as a starting point for exploring potential underlying conditions. While its presence may raise concerns, it’s important to remember that not all echogenic stroma signals a serious problem. Through careful evaluation, including additional imaging and diagnostic tests, medical professionals can effectively assess the significance of echogenic stroma and tailor treatment strategies accordingly.
Understanding the nature and potential implications of echogenic stroma empowers patients to actively participate in their healthcare journey, leading to more informed decisions and better outcomes.
General Inquiries
What are the most common causes of echogenic stroma in the ovaries?
Common causes of echogenic stroma in the ovaries include benign cysts, fibroids, and endometriosis. However, it’s crucial to remember that echogenic stroma in the ovaries can also be associated with more serious conditions, such as ovarian cancer. Therefore, further evaluation and diagnostic testing are essential for a definitive diagnosis.
Is echogenic stroma always a sign of something serious?
No, echogenic stroma is not always a sign of something serious. In many cases, it may be a normal finding or indicate a benign condition. However, it’s important to consult with a healthcare professional for proper evaluation and diagnosis.
What are the potential complications associated with echogenic stroma?
Potential complications associated with echogenic stroma depend on the underlying cause. For example, echogenic stroma in the ovaries can lead to pain, infertility, or even ovarian cancer. However, with timely diagnosis and appropriate treatment, many complications can be prevented or managed effectively.
How often is echogenic stroma found on ultrasound scans?
The frequency of echogenic stroma on ultrasound scans varies depending on the organ or tissue being examined and the patient’s individual health history. It’s important to note that echogenic stroma is not always a significant finding and may be a normal variant in some cases.





