What is corneal stroma? Imagine a windowpane, perfectly clear, allowing light to pass through effortlessly. This is the corneal stroma, a vital component of your eye, ensuring the clarity and sharpness of your vision. It’s a complex, intricately woven structure, a testament to the wonders of nature, playing a crucial role in maintaining the eye’s shape and transparency.
This intricate network of collagen fibers, embedded within a matrix of specialized cells called keratocytes, acts as the eye’s structural foundation. It’s a delicate balance, a symphony of cells and molecules working in harmony, to ensure that light travels unimpeded, reaching the retina for processing into the images we see.
Introduction to the Corneal Stroma
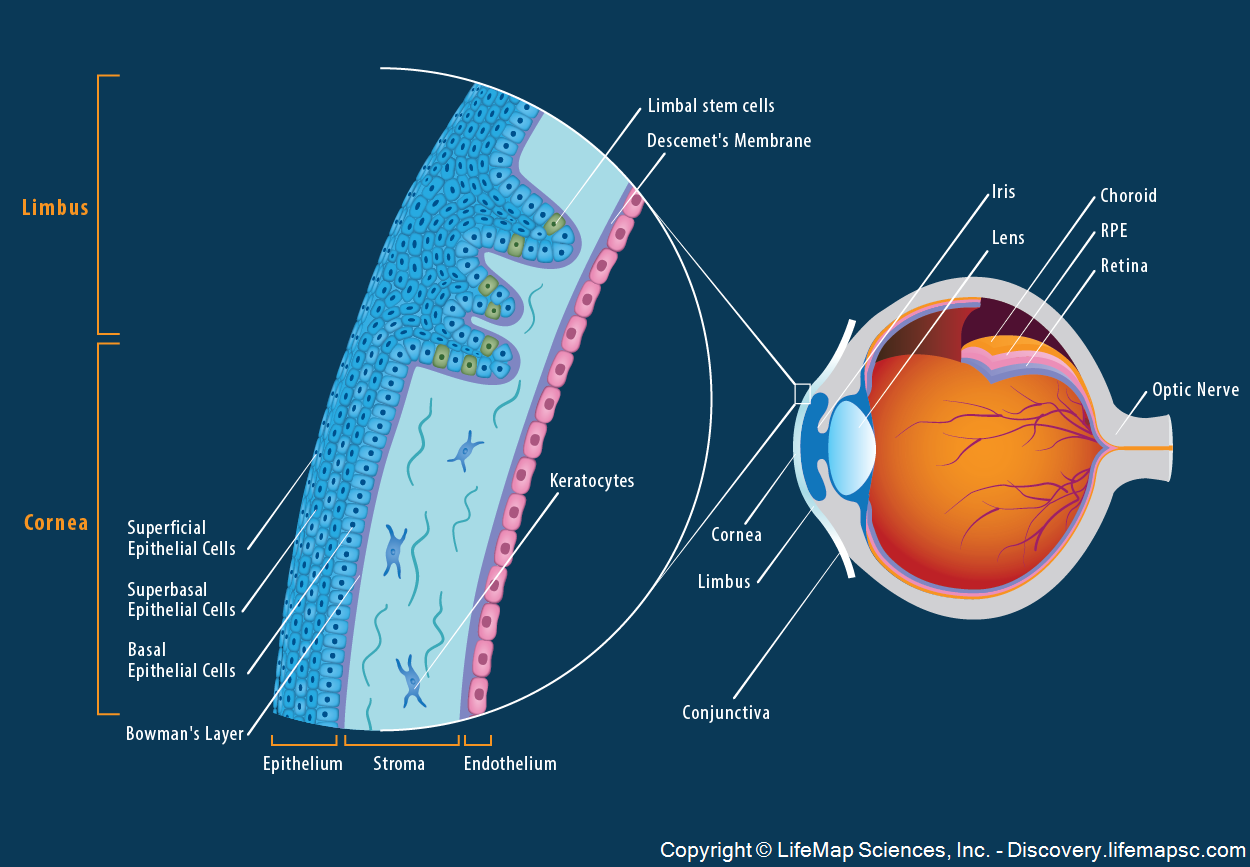
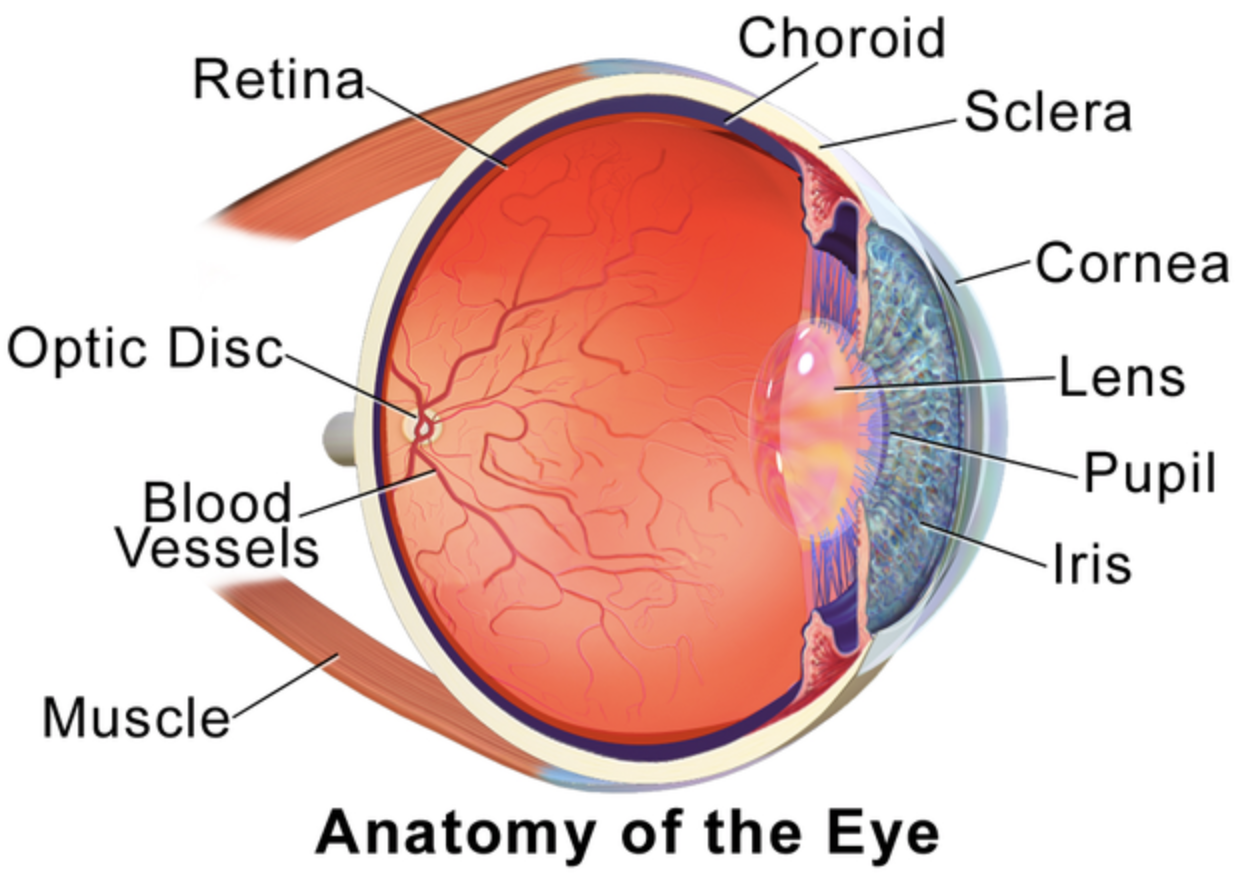
The corneal stroma is the middle layer of the cornea, the transparent front part of the eye. It plays a vital role in maintaining the eye’s shape and transparency, ensuring clear vision.The corneal stroma’s structure is remarkably organized, contributing to its unique properties. It is composed of densely packed collagen fibers, embedded within an extracellular matrix. These fibers are arranged in a precise, parallel fashion, creating a lattice-like structure.
This arrangement is essential for the cornea’s strength and resilience, allowing it to withstand pressure and maintain its shape.
Composition of the Corneal Stroma
The corneal stroma is a complex structure, consisting of:
- Collagen Fibers: These fibers are the primary structural components of the stroma, accounting for about 90% of its dry weight. They are organized into lamellae, thin sheets that are stacked parallel to each other. This layered structure provides strength and flexibility to the cornea.
- Keratocytes: These cells are responsible for producing and maintaining the collagen fibers and the extracellular matrix. They are scattered throughout the stroma and play a crucial role in its repair and regeneration.
- Extracellular Matrix: This is a complex network of proteins and other molecules that surrounds the collagen fibers and keratocytes. It provides hydration and lubrication to the stroma, facilitating the diffusion of nutrients and waste products.
Importance of the Stromal Structure for Light Transmission
The highly organized structure of the corneal stroma is crucial for its transparency, which is essential for light transmission to the retina. The parallel arrangement of collagen fibers minimizes light scattering, ensuring that most of the light entering the eye reaches the retina without distortion.
- Regularity of Collagen Fibers: The precise arrangement of collagen fibers in the stroma ensures that light passes through it with minimal scattering. Any irregularities in the arrangement can lead to light scattering, causing blurred vision.
- Hydration of the Stroma: The extracellular matrix maintains the appropriate hydration level of the stroma, which is essential for its transparency. Dehydration can cause the collagen fibers to shrink, increasing light scattering and reducing clarity.
Collagen Fiber Organization and Structure: What Is Corneal Stroma
The corneal stroma is a highly organized and robust structure, primarily composed of collagen fibers. These fibers are arranged in a precise and intricate manner, contributing significantly to the cornea’s transparency, strength, and overall function. Understanding the organization and structure of these collagen fibers is crucial for appreciating the cornea’s unique properties and its role in vision.
Collagen Fiber Types and Arrangement
The corneal stroma is primarily composed of type I collagen, accounting for approximately 90% of its dry weight. Type I collagen is a fibrous protein that forms long, thin fibrils. These fibrils are arranged in a highly organized and parallel manner, forming lamellae. Each lamella is a thin sheet of collagen fibrils, with the fibrils within each lamella oriented in a specific direction.
Adjacent lamellae have their fibrils oriented at slightly different angles, creating a complex and interwoven structure.This unique arrangement of collagen fibers in the corneal stroma is crucial for its transparency. The parallel arrangement of collagen fibrils within each lamella minimizes light scattering, allowing light to pass through the cornea with minimal distortion. The alternating orientation of fibrils in adjacent lamellae further reduces light scattering by creating a smooth transition between lamellae.
Collagen Cross-Linking, What is corneal stroma
The strength and rigidity of the corneal stroma are further enhanced by collagen cross-linking. Collagen cross-linking is a process that involves the formation of covalent bonds between collagen molecules. These bonds create a network of interconnected collagen molecules, strengthening the overall structure of the corneal stroma.There are two main types of collagen cross-links in the corneal stroma:
- Lysyl oxidase-mediated cross-links: These cross-links are formed by the enzyme lysyl oxidase, which catalyzes the oxidation of lysine residues in collagen molecules. This process results in the formation of aldehydes, which then react with other lysine residues to form cross-links.
- Non-enzymatic cross-links: These cross-links are formed spontaneously through reactions between sugars and collagen molecules. This process, known as glycation, leads to the formation of advanced glycation end products (AGEs), which can contribute to the stiffening of the cornea.
Collagen cross-linking plays a crucial role in maintaining the corneal stroma’s integrity and its ability to withstand the stresses of blinking and eye movements.
Comparison of Collagen Fiber Types
| Type | Composition | Function ||—|—|—|| Type I | 90% of corneal stroma | Provides structural support, maintains transparency || Type V | Minor component | Regulates collagen fibril assembly and diameter || Type VI | Minor component | Forms a network that connects collagen fibrils to other corneal components |
Keratocytes and their Function
Keratocytes are the primary cells of the corneal stroma. These fibroblast-like cells are responsible for maintaining the structural integrity of the stroma and play a crucial role in wound healing.
Role of Keratocytes in Maintaining the Stromal Matrix
Keratocytes are essential for maintaining the stromal matrix by continuously synthesizing and degrading collagen fibers, the primary structural component of the cornea. This dynamic balance ensures the cornea’s transparency and structural integrity.
Role of Keratocytes in Collagen Synthesis and Degradation
Keratocytes synthesize collagen type I, the most abundant collagen in the corneal stroma, and other extracellular matrix components, such as proteoglycans and glycoproteins. They also express enzymes that degrade collagen, such as matrix metalloproteinases (MMPs). This constant synthesis and degradation of collagen is critical for maintaining the proper organization and density of the stromal matrix, which is essential for corneal transparency.
Keratocyte Activation and Proliferation
Keratocytes are quiescent cells that become activated in response to injury or inflammation. This activation triggers a cascade of cellular events, including:
- Increased production of growth factors and cytokines.
- Enhanced expression of collagen and other extracellular matrix proteins.
- Migration of keratocytes to the site of injury.
- Proliferation of keratocytes to repair the damaged tissue.
Keratocyte activation and proliferation are essential for wound healing and the restoration of corneal transparency. However, dysregulation of these processes can lead to scarring and opacity.
Keratocytes are essential for maintaining the structural integrity of the cornea and play a crucial role in wound healing. Their ability to synthesize and degrade collagen, as well as their activation and proliferation in response to injury, are essential for corneal health.
Extracellular Matrix Components
The corneal stroma, as the primary structural component of the cornea, is composed of a complex extracellular matrix (ECM). This intricate network of molecules provides the cornea with its unique biomechanical properties, including its transparency, resilience, and ability to maintain its shape.
Components of the Stromal Extracellular Matrix
The ECM of the corneal stroma is a highly organized and specialized structure, comprising a variety of essential components. These components work in concert to provide the stroma with its remarkable properties.
- Collagen Fibrils: Collagen fibrils, primarily type I collagen, form the primary structural framework of the stroma. These fibrils are arranged in a highly organized, parallel fashion, contributing to the cornea’s tensile strength and resistance to deformation.
- Proteoglycans: Proteoglycans are large, complex molecules composed of a protein core to which glycosaminoglycans (GAGs) are attached. They play a crucial role in maintaining the hydration and transparency of the stroma. The most abundant proteoglycan in the stroma is keratan sulfate (KS), which is responsible for attracting water molecules and maintaining the stromal hydration.
- Glycosaminoglycans (GAGs): GAGs are long, unbranched polysaccharide chains that are highly negatively charged. This negative charge attracts water molecules, contributing to the hydration of the stroma. GAGs also help to regulate the diffusion of nutrients and waste products within the stroma.
- Other ECM Proteins: In addition to collagen and proteoglycans, the stromal ECM contains a variety of other proteins, including fibronectin, laminin, and elastin. These proteins contribute to the structural integrity and organization of the ECM, as well as cell adhesion and signaling.
Role of Proteoglycans and Glycosaminoglycans in Maintaining Stromal Hydration and Transparency
The hydration of the corneal stroma is crucial for maintaining its transparency. The unique composition of the ECM, particularly the presence of proteoglycans and GAGs, plays a vital role in this process. The negative charges of GAGs attract water molecules, creating a hydrated environment within the stroma. This hydration is essential for the proper function of the corneal stroma, as it allows for the diffusion of nutrients and waste products, and maintains the appropriate refractive index for light transmission.
Importance of the Stromal Matrix for Cell Signaling and Communication
The stromal ECM is not merely a passive structural scaffold but also actively participates in cell signaling and communication. The various components of the ECM, including collagen, proteoglycans, and other ECM proteins, interact with keratocytes, the resident cells of the stroma, through specific receptors. This interaction influences keratocyte behavior, including proliferation, differentiation, and matrix synthesis. The ECM also plays a role in the wound healing process, guiding the migration and differentiation of cells involved in repair.
Corneal Stroma Development and Growth
The corneal stroma, the transparent, collagen-rich middle layer of the cornea, undergoes a complex developmental process from its initial formation during embryogenesis to its mature state in adulthood. This process involves intricate interactions between various cellular and molecular components, resulting in a highly organized and functional structure that plays a crucial role in maintaining corneal transparency and refractive power.
Stages of Corneal Stroma Development
The development of the corneal stroma can be broadly divided into several stages, each characterized by distinct cellular and molecular events.
- Embryonic Stage (Weeks 5-8): The corneal stroma originates from the neural crest cells, which migrate from the developing brain to the surface ectoderm of the eye. These cells differentiate into keratocytes, the primary stromal cell type, and begin to synthesize and deposit collagen fibrils, forming a loose, disorganized stromal matrix.
- Fetal Stage (Weeks 9-40): During this stage, the stromal matrix undergoes significant growth and organization. Keratocytes continue to produce and deposit collagen fibrils, which assemble into lamellae, thin, parallel layers of collagen fibers. These lamellae are arranged in a highly organized, alternating pattern, contributing to the transparency of the cornea. The stromal thickness increases significantly, and the stromal matrix becomes more compact and organized.
- Postnatal Stage (Birth to Adulthood): After birth, the corneal stroma continues to mature, with ongoing collagen deposition and organization. The lamellae become more tightly packed, and the stromal matrix becomes more rigid and resistant to deformation. This process contributes to the stability and structural integrity of the cornea.
Mechanisms of Stromal Growth and Maturation
The growth and maturation of the corneal stroma are driven by a complex interplay of cellular and molecular mechanisms, including:
- Collagen Synthesis and Deposition: Keratocytes are responsible for synthesizing and depositing collagen fibrils, the primary structural component of the stromal matrix. The type I collagen, which comprises about 90% of the stromal collagen, is assembled into fibrils, which then organize into lamellae. The regulation of collagen synthesis and deposition is influenced by various growth factors and signaling pathways, ensuring the precise organization and thickness of the stromal matrix.
- Extracellular Matrix Assembly: The collagen fibrils are embedded in an extracellular matrix, which consists of other structural proteins, proteoglycans, and water. These components interact with collagen fibrils, contributing to the mechanical properties and transparency of the stromal matrix. The organization and composition of the extracellular matrix are tightly regulated, ensuring the proper function and integrity of the cornea.
- Stromal Cell Interactions: Keratocytes interact with each other and with the extracellular matrix, influencing the growth and organization of the stromal matrix. These interactions involve various signaling molecules and adhesion proteins, which regulate cell migration, proliferation, and differentiation, contributing to the development and maintenance of the stromal structure.
Timeline of Corneal Stromal Development
| Stage | Timeline | Key Events |
|---|---|---|
| Embryonic | Weeks 5-8 | Neural crest cell migration, keratocyte differentiation, initial collagen deposition, formation of loose stromal matrix |
| Fetal | Weeks 9-40 | Stromal matrix growth, lamellae formation, increased stromal thickness, compact and organized stromal matrix |
| Postnatal | Birth to Adulthood | Continued collagen deposition and organization, tightly packed lamellae, rigid and resistant stromal matrix |
Clinical Significance of the Corneal Stroma
The corneal stroma, the thickest layer of the cornea, plays a crucial role in maintaining the eye’s structural integrity and optical clarity. Any abnormalities within the stroma can significantly impact visual function and overall eye health. These abnormalities can range from subtle changes in collagen organization to severe inflammatory conditions, leading to a spectrum of visual impairments and potential complications.
Impact of Stromal Abnormalities on Visual Function and Eye Health
The corneal stroma’s unique structure, characterized by highly organized collagen fibers, contributes significantly to the cornea’s transparency and refractive properties. Any disruption to this delicate arrangement can affect light transmission and distort vision. For instance, swelling of the stroma due to inflammation or edema can cause blurring or haziness, reducing visual acuity. Additionally, changes in collagen density or fiber alignment can lead to irregular corneal shape, resulting in astigmatism and distorted vision.
Examples of Corneal Stromal Diseases and their Associated Symptoms
Various diseases and conditions can affect the corneal stroma, leading to a range of symptoms. Some common examples include:
Keratoconus
- Cause: A progressive corneal disorder characterized by thinning and protrusion of the central cornea, leading to a cone-like shape.
- Symptoms: Blurred vision, distorted images, increased sensitivity to light, and frequent changes in eyeglass prescriptions.
Fuchs’ Endothelial Dystrophy
- Cause: A genetic disorder affecting the corneal endothelium, the innermost layer of the cornea, which pumps fluid out of the stroma. This dysfunction leads to stromal edema and thickening.
- Symptoms: Blurred vision, sensitivity to light, and gradual loss of vision.
Corneal Edema
- Cause: Swelling of the corneal stroma due to fluid accumulation, often caused by conditions affecting the endothelium, inflammation, or trauma.
- Symptoms: Blurred vision, halos around lights, and a feeling of grittiness in the eye.
Corneal Scarring
- Cause: Formation of scar tissue in the stroma due to trauma, infection, or inflammation. Scar tissue is opaque and can significantly impair vision.
- Symptoms: Blurred vision, distorted images, and reduced visual acuity.
Stromal Disorders, Causes, and Treatment Options
| Disorder | Causes | Treatment Options |
|---|---|---|
| Keratoconus | Genetic predisposition, eye rubbing, and connective tissue disorders | Contact lenses, corneal cross-linking, corneal transplantation |
| Fuchs’ Endothelial Dystrophy | Genetic predisposition | Contact lenses, corneal transplantation, Descemet’s stripping automated endothelial keratoplasty (DSAEK) |
| Corneal Edema | Endothelial dysfunction, inflammation, trauma | Treatment of underlying cause, topical medications, corneal transplantation |
| Corneal Scarring | Trauma, infection, inflammation | Antibiotics, anti-inflammatory medications, corneal transplantation |
Research and Future Directions
The corneal stroma, as the primary structural component of the cornea, is a fascinating area of ongoing research. Understanding its intricate biology and regenerative potential holds significant promise for treating corneal stromal disorders and improving vision for millions worldwide.
Current Research Trends in Corneal Stroma Biology and Regenerative Medicine
Current research in corneal stroma biology focuses on various aspects, including the intricate interplay between keratocytes and the extracellular matrix, the role of stem cells in corneal stromal regeneration, and the development of bioengineered corneal tissues. These areas are driving advancements in regenerative medicine for corneal disorders.
- Keratocyte Biology and Extracellular Matrix Interactions: Researchers are investigating the molecular mechanisms that regulate keratocyte function and their interaction with the extracellular matrix. This includes studying the role of growth factors, cytokines, and mechanical forces in modulating keratocyte behavior and influencing corneal stromal homeostasis.
- Stem Cell Therapy for Corneal Stroma Regeneration: Stem cell therapy holds significant promise for corneal stromal regeneration. Researchers are exploring the potential of various stem cell sources, including limbal stem cells, mesenchymal stem cells, and induced pluripotent stem cells, to regenerate corneal stroma and restore corneal function.
- Bioengineered Corneal Tissues: Bioengineering approaches are being developed to create artificial corneal tissues that can be used for transplantation. These approaches involve using biocompatible materials, such as collagen, to create scaffolds that can be seeded with keratocytes or other cell types. These bioengineered tissues have the potential to overcome the limitations of donor corneal tissue availability and address the increasing demand for corneal transplantation.
Challenges and Opportunities in Understanding and Treating Corneal Stromal Disorders
While significant progress has been made in understanding corneal stromal biology, several challenges remain in effectively treating corneal stromal disorders. These challenges present opportunities for future research and innovation.
- Scarring and Fibrosis: Scarring and fibrosis are major complications of corneal stromal injuries and diseases. Understanding the mechanisms underlying these processes and developing strategies to prevent or reverse scarring is crucial for preserving corneal transparency and vision.
- Immune Rejection: Corneal transplantation, a common treatment for severe corneal disorders, is often limited by immune rejection. Research is focused on developing strategies to reduce immune rejection, such as using immunosuppressive drugs or developing immune-privileged corneal grafts.
- Limited Donor Tissue Availability: The availability of donor corneal tissue remains a significant challenge for corneal transplantation. Bioengineering approaches and stem cell therapy hold the potential to overcome this limitation by providing alternative sources of corneal tissue.
Potential Future Directions for Research in Corneal Stroma Regeneration and Transplantation
Future research in corneal stroma regeneration and transplantation will focus on addressing the current challenges and exploring novel approaches. These areas represent promising avenues for advancing the field and improving patient outcomes.
- Development of Biocompatible and Biodegradable Scaffolds: Developing biocompatible and biodegradable scaffolds that can mimic the natural extracellular matrix of the corneal stroma is crucial for supporting cell growth and tissue regeneration. These scaffolds should provide structural support, promote cell adhesion and differentiation, and facilitate the formation of a functional corneal stroma.
- Gene Therapy for Corneal Stroma Regeneration: Gene therapy offers a promising approach for treating corneal stromal disorders by targeting specific genes involved in corneal stromal development, regeneration, or disease pathogenesis. This approach may involve delivering genes that promote keratocyte function, inhibit fibrosis, or enhance immune tolerance.
- Personalized Medicine for Corneal Stroma Regeneration: Personalized medicine approaches, tailored to individual patients’ genetic and clinical characteristics, can improve the effectiveness of corneal stromal regeneration strategies. These approaches may involve using patient-specific stem cells, developing personalized bioengineered corneal tissues, or optimizing gene therapy strategies based on individual genetic profiles.
The corneal stroma, with its delicate architecture and vital functions, is a marvel of biological engineering. Its intricate structure and dynamic interplay of cells and molecules ensure the clarity of our vision, allowing us to experience the world in all its vibrant detail. Understanding this fascinating component of the eye opens a window into the complex world of vision, paving the way for advancements in treating and preventing corneal disorders.
Common Queries
What happens if the corneal stroma is damaged?
Damage to the corneal stroma can lead to various issues, including impaired vision, scarring, and even vision loss. The severity depends on the extent and nature of the damage.
Can the corneal stroma regenerate?
The corneal stroma has a limited capacity for regeneration. However, research is ongoing to explore potential strategies for enhancing its regenerative potential.
Are there any conditions that specifically affect the corneal stroma?
Yes, there are several conditions that can affect the corneal stroma, including keratoconus, corneal dystrophies, and corneal ulcers. These conditions can lead to a range of visual impairments.






