What is echogenic stroma in ovary – What is echogenic stroma in the ovary? This intriguing question delves into the realm of ovarian health, where ultrasound imaging reveals a fascinating and often perplexing phenomenon. Echogenic stroma, characterized by its bright, reflective appearance on ultrasound, can be a sign of normal ovarian function or a potential indicator of underlying conditions. It’s a topic that sparks curiosity and prompts us to explore the intricate world of the female reproductive system.
Echogenic stroma, often referred to as “bright spots” or “white spots” on ultrasound, is a common finding in women of all ages. It refers to the dense, fibrous tissue that makes up the ovarian stroma, the supporting framework of the ovary. While often benign, echogenic stroma can sometimes be associated with various conditions, including polycystic ovary syndrome (PCOS), endometriosis, and even ovarian cancer.
Understanding the causes, implications, and management of echogenic stroma is crucial for women’s reproductive health.
What is Echogenic Stroma?
Echogenic stroma, a term frequently encountered in ultrasound reports, refers to a specific appearance of the ovarian tissue. It is a common finding, often detected during routine pelvic ultrasounds. Understanding its nature and significance is crucial for interpreting ultrasound findings and evaluating ovarian health.
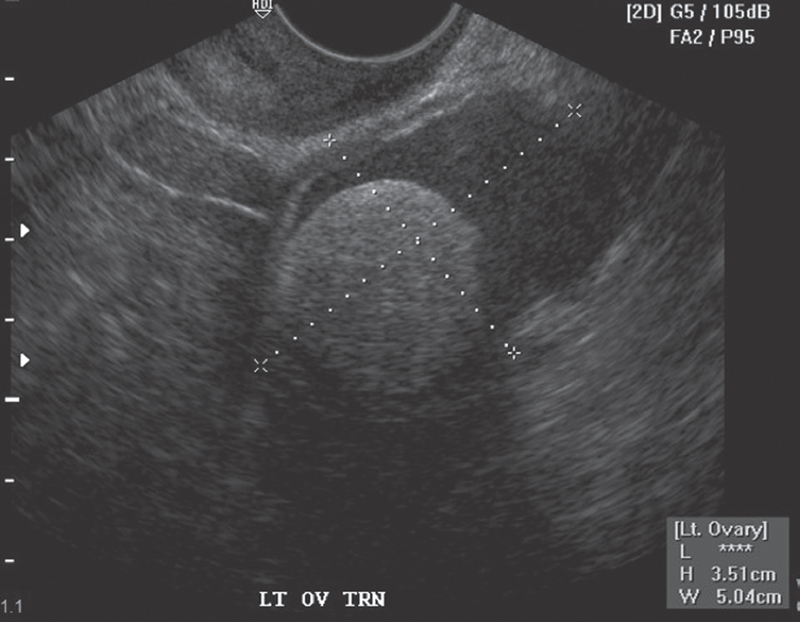
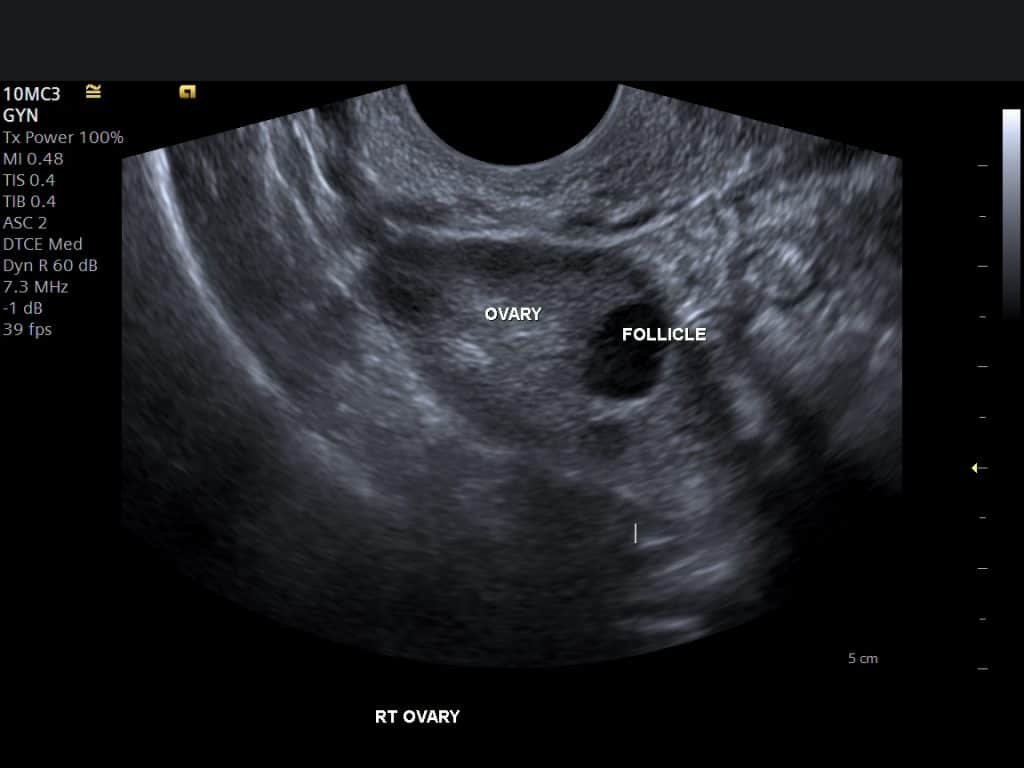
Appearance on Ultrasound
Echogenic stroma is characterized by a bright, white, or hyperechoic appearance on ultrasound images. This brightness is due to the increased density of the ovarian stroma, the tissue that surrounds the follicles and the ovary’s outer layer. In contrast, normal ovarian stroma usually appears as a darker, less reflective area on ultrasound.
Significance in Ovarian Health
Echogenic stroma can be a sign of various conditions, some benign and others potentially concerning. Its significance depends on several factors, including:
- Age: Echogenic stroma is more common in women approaching menopause. The ovarian stroma becomes denser and more echogenic as estrogen levels decline.
- Location: Echogenic stroma can be localized to a specific area of the ovary or diffuse throughout the entire ovary.
- Size: Small, isolated areas of echogenic stroma are generally considered benign. However, large areas or those associated with other abnormalities may warrant further investigation.
Example: A 45-year-old woman undergoing a routine ultrasound may show scattered areas of echogenic stroma in her ovaries. This is a common finding in women approaching menopause and is usually considered benign. However, if the echogenic stroma is extensive or accompanied by other findings like cysts or masses, further investigation might be necessary.
Benign Conditions
Echogenic stroma can be associated with various benign conditions, including:
- Normal aging: As mentioned earlier, the ovarian stroma naturally becomes denser and more echogenic with age.
- Polycystic Ovarian Syndrome (PCOS): In women with PCOS, the ovaries often have a thickened, echogenic stroma, sometimes accompanied by multiple small cysts.
- Fibroids: While not directly related to the ovaries, fibroids in the uterus can sometimes appear as echogenic structures adjacent to the ovaries.
Potentially Concerning Conditions
While echogenic stroma is often benign, it can also be associated with certain potentially concerning conditions:
- Ovarian tumors: Some ovarian tumors, particularly those of stromal origin, can appear as echogenic masses on ultrasound.
- Ovarian cancer: While rare, ovarian cancer can sometimes manifest as echogenic areas in the ovary.
- Endometriosis: Endometriosis, a condition where endometrial tissue grows outside the uterus, can sometimes present as echogenic lesions in the ovaries.
Note: It is important to emphasize that echogenic stroma alone does not necessarily indicate a serious condition. However, its presence should be considered in conjunction with other clinical and ultrasound findings.
Further Evaluation
If an ultrasound reveals echogenic stroma, the doctor may recommend further evaluation depending on the patient’s age, symptoms, and other ultrasound findings. These evaluations may include:
- Repeat ultrasound: A follow-up ultrasound can help monitor any changes in the echogenic stroma over time.
- Blood tests: Blood tests can assess hormone levels and other markers that may provide further insights into ovarian function and health.
- MRI: In some cases, an MRI scan may be recommended to provide more detailed images of the ovaries and surrounding structures.
Causes of Echogenic Stroma: What Is Echogenic Stroma In Ovary

Echogenic stroma, a phenomenon often observed in ultrasound imaging of the ovaries, can be attributed to various factors. The appearance of echogenic stroma can vary, ranging from subtle echoes to a completely solid, white appearance. Understanding the potential causes behind this finding is crucial for accurate diagnosis and appropriate management.
Age and Hormonal Factors, What is echogenic stroma in ovary
Age plays a significant role in the development of echogenic stroma. As women approach menopause, the ovaries undergo natural changes, including a decrease in estrogen production. This hormonal shift can lead to increased collagen deposition within the ovarian stroma, resulting in the echogenic appearance on ultrasound.
Medical Conditions
Certain medical conditions can also contribute to the presence of echogenic stroma in the ovaries. These conditions often involve hormonal imbalances or changes in ovarian tissue structure.
- Polycystic Ovarian Syndrome (PCOS): PCOS is a common hormonal disorder characterized by irregular periods, excess androgen production, and the development of multiple cysts on the ovaries. The cysts associated with PCOS can sometimes appear as echogenic stroma on ultrasound.
- Ovarian Hyperstimulation Syndrome (OHSS): OHSS is a potential complication of fertility treatments involving the use of hormones to stimulate egg production. The overstimulation of the ovaries can lead to fluid accumulation and inflammation, which may appear as echogenic stroma on ultrasound.
- Endometriosis: Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, including the ovaries. The presence of endometriosis can sometimes cause echogenic stroma in the ovaries.
- Fibroids: While fibroids are primarily found in the uterus, they can occasionally occur in the ovaries. These benign tumors can appear as echogenic masses on ultrasound.
Clinical Implications of Echogenic Stroma
Echogenic stroma, while often a benign finding, can have important clinical implications, particularly in the context of female reproductive health. Understanding its potential impact on fertility and other ovarian conditions is crucial for guiding patient care and management.
Relationship to Infertility and Reproductive Challenges
The presence of echogenic stroma in the ovary can be associated with infertility or reproductive challenges, although the exact mechanism is not fully understood. Some studies suggest that echogenic stroma may be associated with:
- Ovarian dysfunction: Echogenic stroma may indicate changes in the ovarian microenvironment, potentially affecting ovulation and egg quality. This can contribute to difficulties in achieving pregnancy.
- Increased risk of miscarriage: Some research suggests that echogenic stroma may be linked to a higher risk of miscarriage, although more research is needed to confirm this association.
- Reduced ovarian reserve: Echogenic stroma may be a sign of diminished ovarian reserve, which is a decrease in the number and quality of eggs available for fertilization. This can impact fertility potential.
It’s important to note that the presence of echogenic stroma does not automatically mean infertility or reproductive challenges. Many women with echogenic stroma have healthy pregnancies, and other factors, such as age, lifestyle, and underlying medical conditions, can also influence fertility.
Potential Marker for Other Ovarian Conditions
Echogenic stroma can sometimes be a marker for other ovarian conditions, such as:
- Polycystic ovary syndrome (PCOS): Echogenic stroma is often seen in women with PCOS, a hormonal disorder that can affect ovulation and increase the risk of infertility. This association is based on the observation that echogenic stroma is frequently found in women with PCOS, but it is not a definitive diagnostic criterion.
- Ovarian fibroids: Echogenic stroma can be seen in the presence of ovarian fibroids, benign growths in the ovary. However, echogenic stroma itself is not a fibroid, and further evaluation may be needed to confirm the diagnosis.
- Endometriosis: While less common, echogenic stroma can sometimes be associated with endometriosis, a condition where uterine tissue grows outside the uterus. This association is based on observations that echogenic stroma can be seen in some women with endometriosis, but more research is needed to understand the relationship.
The presence of echogenic stroma should prompt further investigation to rule out other potential ovarian conditions, especially if accompanied by other symptoms or findings.
Diagnosis and Management
The diagnosis of echogenic stroma typically involves a combination of clinical evaluation and imaging studies. The process aims to identify the presence of echogenic stroma, assess its characteristics, and rule out other potential causes of similar findings.
Ultrasound Imaging
Ultrasound imaging plays a pivotal role in the diagnosis of echogenic stroma. Transvaginal ultrasound, a technique that uses a probe inserted into the vagina, provides detailed images of the ovaries. The presence of echogenic areas within the ovarian stroma can be readily identified on ultrasound. The sonographer meticulously examines the ovarian structure, noting the size, shape, and echogenicity of the echogenic areas.
They also look for any associated abnormalities, such as cysts or masses.
Other Diagnostic Tests
In some cases, additional diagnostic tests may be necessary to confirm the diagnosis of echogenic stroma or to evaluate any associated conditions. These tests may include:
- Pelvic Magnetic Resonance Imaging (MRI): MRI can provide more detailed images of the ovaries and surrounding tissues, which can help to further characterize the echogenic stroma and rule out other possibilities.
- Blood Tests: Blood tests may be performed to assess hormone levels and to check for any signs of inflammation or infection.
- Biopsy: In rare cases, a biopsy may be necessary to obtain a tissue sample for microscopic examination. This is typically done when the echogenic stroma is associated with other abnormalities or when there is a concern for malignancy.
Treatment Options
The management of echogenic stroma depends on the individual’s clinical presentation, the size and characteristics of the echogenic areas, and the presence of any associated symptoms.
Observation
For many women with echogenic stroma, particularly those with small, asymptomatic lesions, observation may be the most appropriate approach. Regular ultrasound monitoring allows for the assessment of any changes in the size or appearance of the echogenic areas over time. This approach is typically employed when the echogenic stroma is deemed to be benign and not associated with any other complications.
Surgical Intervention
Surgical intervention may be considered in certain situations, such as:
- Large or rapidly growing echogenic areas: If the echogenic areas are large or growing rapidly, surgical intervention may be recommended to rule out malignancy and to alleviate any associated symptoms.
- Symptoms: If the echogenic stroma is causing pain or other symptoms, surgery may be considered to address the underlying cause.
- Concerns about malignancy: If there is a suspicion of malignancy, surgical intervention is often recommended to obtain a tissue sample for biopsy and to remove the affected tissue.
The surgical procedure typically involves laparoscopic or open surgery to remove the affected ovary or a portion of the ovary.
Research and Future Directions
The understanding of echogenic ovarian stroma is evolving, driven by advancements in imaging technologies and a growing interest in its clinical implications. Current research focuses on clarifying the underlying mechanisms, refining diagnostic approaches, and exploring potential therapeutic interventions.
Understanding the Mechanisms of Echogenic Stroma
The exact mechanisms underlying the development of echogenic ovarian stroma remain under investigation. Current research aims to unravel the complex interplay of factors contributing to its formation, including:
- Cellular and Molecular Changes: Studies are investigating alterations in ovarian stromal cell composition, proliferation, and apoptosis, as well as the role of specific genes and proteins involved in these processes.
- Hormonal Influences: Research explores the influence of sex hormones, particularly estrogen and progesterone, on stromal cell behavior and the development of echogenic stroma. This includes examining the potential impact of hormonal imbalances and fluctuations.
- Vascular Factors: Investigations focus on the role of vascularization in echogenic stroma formation, including changes in blood flow, angiogenesis, and the presence of microvascular abnormalities.
Improving Diagnostic Accuracy
While ultrasound is the primary diagnostic tool for echogenic stroma, ongoing research seeks to enhance its accuracy and specificity. This involves:
- Developing Standardized Criteria: Researchers are working to establish standardized criteria for ultrasound interpretation, incorporating features like echogenicity, size, location, and morphology, to improve consistency in diagnosis.
- Exploring Advanced Imaging Techniques: Studies are exploring the potential of advanced imaging modalities, such as magnetic resonance imaging (MRI) and Doppler ultrasound, to provide more detailed information about the ovarian stroma and differentiate echogenic stroma from other conditions.
- Utilizing Biomarkers: Researchers are investigating the potential of specific biomarkers, detectable in blood or tissue, to aid in the diagnosis and monitoring of echogenic stroma.
Novel Therapeutic Approaches
Current management of echogenic stroma is primarily focused on observation and monitoring. However, ongoing research explores potential therapeutic interventions, including:
- Hormonal Therapy: Studies are investigating the efficacy of hormonal therapies, such as oral contraceptives or gonadotropin-releasing hormone (GnRH) agonists, in managing echogenic stroma and its associated symptoms.
- Targeted Therapies: Research explores the potential of targeted therapies, such as drugs that inhibit specific signaling pathways involved in stromal cell proliferation or angiogenesis, to treat echogenic stroma.
- Minimally Invasive Surgical Techniques: Studies are evaluating the effectiveness and safety of minimally invasive surgical techniques, such as laparoscopic cystectomy or oophorectomy, in managing echogenic stroma, particularly in cases of large or symptomatic lesions.
Echogenic stroma in the ovary, though often a benign finding, underscores the importance of regular gynecological checkups and comprehensive ultrasound imaging. By understanding the potential causes, implications, and management strategies, women can make informed decisions about their reproductive health. As research continues to unravel the complexities of this phenomenon, we can expect even greater insights into the intricate workings of the ovary and the role of echogenic stroma in women’s overall well-being.
Frequently Asked Questions
What are the common symptoms associated with echogenic stroma in the ovary?
Echogenic stroma itself doesn’t typically cause noticeable symptoms. However, if it’s associated with conditions like PCOS, endometriosis, or ovarian cysts, you might experience irregular periods, pelvic pain, or difficulty conceiving.
Is echogenic stroma always a cause for concern?
Not necessarily. In many cases, echogenic stroma is a benign finding and doesn’t require treatment. However, it’s essential to consult with your doctor for proper evaluation and management based on your individual circumstances.
What are the long-term implications of echogenic stroma?
The long-term implications depend on the underlying cause and associated conditions. If it’s benign, it usually doesn’t affect your overall health or reproductive potential. However, if it’s associated with conditions like PCOS or endometriosis, it can have implications for fertility and menstrual cycles.
Can echogenic stroma be treated?
Treatment depends on the underlying cause and severity of the condition. If it’s benign, observation may be sufficient. If it’s associated with other conditions, treatment will focus on addressing those underlying factors.






