Does lobular carcinoma in situ invade stroma? This is a question that often arises when discussing breast cancer and its various forms. Lobular carcinoma in situ (LCIS) is a non-invasive form of breast cancer, meaning it hasn’t spread beyond the milk ducts or lobules of the breast. While it doesn’t directly invade surrounding tissue, LCIS is considered a precursor to invasive breast cancer, making it a significant concern for many women.
Understanding the nature of LCIS and its relationship to the surrounding stroma is crucial for effective diagnosis, treatment, and prevention. This article will delve into the characteristics of LCIS, the role of stroma in breast health, and the critical distinction between in situ and invasive cancer. We will explore the clinical implications of LCIS, including risk factors, management options, and ongoing research aimed at understanding and treating this condition.
Understanding Lobular Carcinoma In Situ (LCIS)
Lobular carcinoma in situ (LCIS) is a non-invasive breast cancer that involves abnormal cells confined to the milk ducts. It is considered a precancerous condition, meaning it can develop into invasive breast cancer. LCIS is a relatively common finding, detected in about 1-2% of breast biopsies.
Characteristics of LCIS
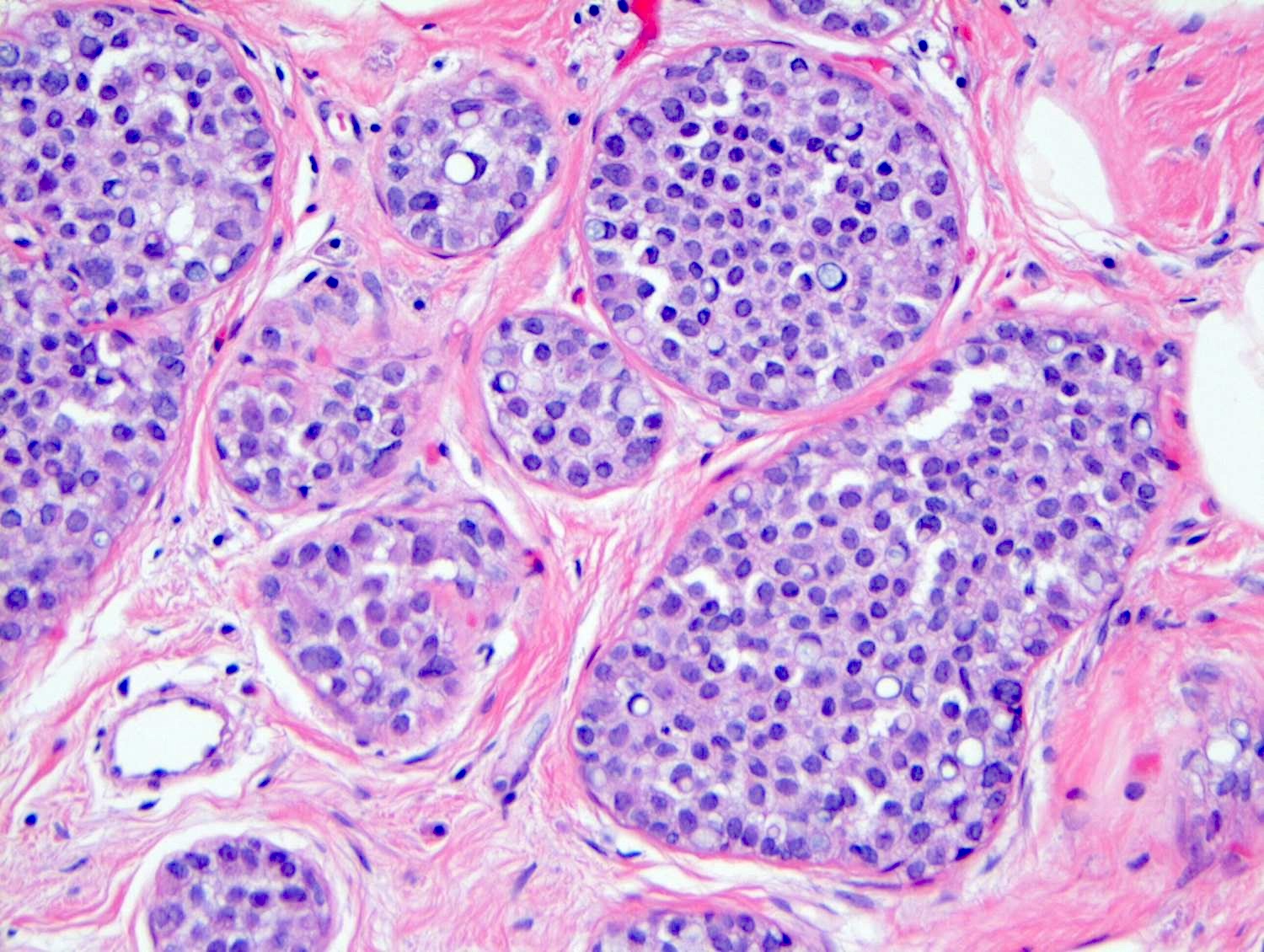
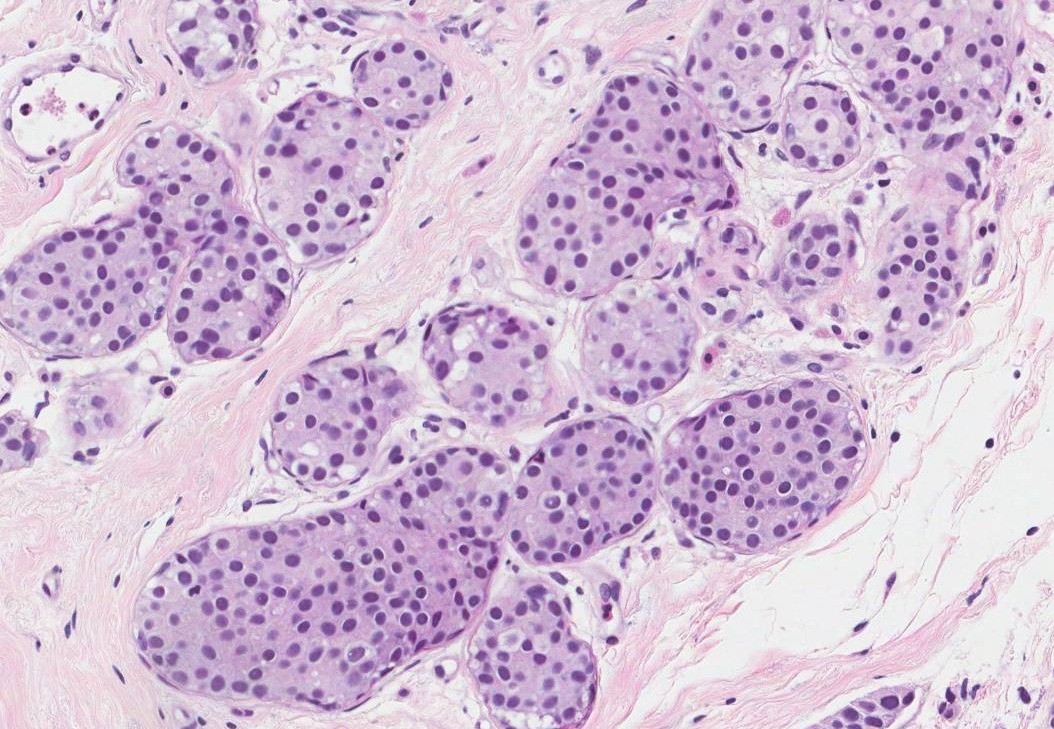
LCIS is characterized by a proliferation of small, round, and tightly packed cells that lack the typical ductal architecture. These cells often exhibit a “single file” pattern, referred to as “lobular” or “Indian file” arrangement. The cells may also exhibit loss of adhesion, leading to a dispersed pattern. These cellular changes, while confined to the milk ducts, are indicative of a potential for malignant transformation.
Significance of LCIS as a Precursor to Invasive Breast Cancer
LCIS is considered a significant risk factor for developing invasive breast cancer. While not all women with LCIS will develop invasive cancer, the risk is increased compared to women without LCIS. The risk of developing invasive breast cancer is influenced by various factors, including age, family history, and genetic mutations.
Subtypes of LCIS and Associated Risks
LCIS can be classified into different subtypes, each with varying risks of progression to invasive cancer. The most common subtypes include:
- Classical LCIS: The most prevalent subtype, characterized by a typical “Indian file” pattern of cells. It is associated with a moderate risk of developing invasive breast cancer.
- Pleomorphic LCIS: This subtype exhibits greater cellular variation, including larger and more irregular cells. It is associated with a higher risk of invasive breast cancer compared to classical LCIS.
- Atypical LCIS: This subtype is considered to be a more aggressive form of LCIS. It is characterized by cells that are more abnormal and have a higher risk of progressing to invasive cancer.
Stroma
The stroma is the supporting tissue that surrounds and interacts with the epithelial cells in the breast. It is a complex network of cells, fibers, and extracellular matrix that plays a crucial role in breast development, function, and health.
Functions of the Stroma
The stroma provides structural support for the breast tissue, enabling its proper shape and organization. It also acts as a conduit for blood vessels and nerves, supplying the epithelial cells with nutrients and oxygen, and allowing for communication between different parts of the breast. The stroma also plays a critical role in regulating breast development, growth, and involution.
Types of Stromal Cells
The stroma is composed of various types of cells, each with specific functions:
- Fibroblasts: These are the most abundant stromal cells and are responsible for producing collagen and other extracellular matrix components, providing structural support and elasticity to the breast tissue. They also contribute to the formation of the basement membrane, a specialized layer that separates the epithelial cells from the stroma.
- Myofibroblasts: These cells are similar to fibroblasts but have the ability to contract, which is important for tissue remodeling and wound healing. Myofibroblasts are also involved in the regulation of breast development and lactation.
- Smooth muscle cells: These cells are found in the walls of blood vessels and lymphatic vessels, and they help to regulate blood flow and lymphatic drainage in the breast.
- Immune cells: The stroma contains various immune cells, such as macrophages, lymphocytes, and mast cells, which play a role in protecting the breast tissue from infections and inflammation.
Extracellular Matrix
The extracellular matrix is the non-cellular component of the stroma, providing a framework for the stromal cells and regulating their behavior. It is composed of various proteins, including collagen, elastin, and laminin, as well as glycosaminoglycans and water. The extracellular matrix plays a crucial role in breast development, tissue repair, and tumorigenesis.
Invasion
The distinction between in situ and invasive cancer lies in the presence or absence of invasion, which refers to the cancer cells’ ability to penetrate the surrounding tissue. While in situ cancer cells remain confined to their original location, invasive cancer cells break free from their original site and spread to nearby tissues.
The Process of Invasion
The invasion process is a complex multi-step process that involves a series of interactions between cancer cells and the surrounding stroma. * Adhesion: Cancer cells must first detach from their original location and adhere to the surrounding stroma.
Degradation
Cancer cells secrete enzymes that break down the extracellular matrix (ECM), the network of proteins that holds cells together.
Migration
Cancer cells move through the ECM, following a trail of chemoattractants.
Proliferation
Cancer cells divide and multiply, forming new colonies in the invaded tissue.
Growth Patterns and Characteristics of LCIS and Invasive Lobular Carcinoma
The growth patterns and characteristics of LCIS and invasive lobular carcinoma differ significantly.
LCIS
- Growth Pattern: LCIS cells typically grow in a cohesive, cluster-like manner, often referred to as “single file” or “Indian file” formation.
- Invasion: LCIS cells remain confined to the milk ducts and do not invade the surrounding stroma.
- Characteristics: LCIS cells often lack the typical features of invasive cancer, such as a distinct border, abnormal cell shape, or increased mitotic activity.
Invasive Lobular Carcinoma
- Growth Pattern: Invasive lobular carcinoma cells often grow in a diffuse, infiltrative pattern, spreading widely through the surrounding tissue.
- Invasion: Invasive lobular carcinoma cells penetrate the basement membrane and invade the surrounding stroma.
- Characteristics: Invasive lobular carcinoma cells typically display features of malignancy, such as a distinct border, abnormal cell shape, and increased mitotic activity.
Clinical Implications of LCIS
Lobular carcinoma in situ (LCIS) is a non-invasive breast cancer that poses a significant clinical challenge due to its potential to progress to invasive cancer. Understanding the clinical implications of LCIS is crucial for guiding patient management and optimizing outcomes.
Clinical Presentation and Diagnosis
LCIS is typically asymptomatic and is often discovered incidentally during routine mammograms or other imaging studies. However, in some cases, patients may present with subtle symptoms such as nipple discharge or breast tenderness. Diagnosis is typically made through a combination of imaging and biopsy. Mammograms may reveal microcalcifications or architectural distortions. Ultrasound may show a suspicious mass or microlobular pattern.
Biopsy is necessary for definitive diagnosis, and the presence of atypical lobular hyperplasia (ALH) or LCIS on biopsy can be indicative of increased risk for future invasive cancer.
Risk Factors Associated with LCIS Progression to Invasive Cancer
While LCIS is a non-invasive condition, it carries a risk of progressing to invasive breast cancer. Several factors have been identified as increasing the risk of progression, including:
- Family History of Breast Cancer: A strong family history of breast cancer, particularly in close relatives, significantly elevates the risk of LCIS progression.
- Age at Diagnosis: Women diagnosed with LCIS at a younger age tend to have a higher risk of progression.
- Multiple Lesions: The presence of multiple LCIS lesions within the breast is associated with an increased risk of invasive cancer.
- High-Grade LCIS: LCIS with high-grade cytological features is considered to be more aggressive and carries a higher risk of progression.
- Genetic Mutations: Certain genetic mutations, such as BRCA1 and BRCA2, are known to increase the risk of both LCIS and invasive breast cancer.
Management Options for LCIS
Management of LCIS is tailored to the individual patient’s risk factors and preferences. Options include:
- Surveillance: Regular mammograms and clinical breast exams are recommended for patients with LCIS to monitor for any changes. The frequency of surveillance is individualized based on risk factors and patient preferences.
- Treatment: Treatment options for LCIS include:
- Tamoxifen: This medication can help reduce the risk of LCIS progression to invasive cancer. It is often prescribed for women with high-risk factors.
- Selective Estrogen Receptor Modulators (SERMs): Similar to tamoxifen, SERMs can reduce the risk of invasive cancer in women with LCIS.
- Prophylactic Mastectomy: This involves surgical removal of the breast tissue where LCIS was found. It is a more aggressive approach and may be considered for women with very high risk factors or a strong preference for reducing their cancer risk.
- Prevention Strategies: While LCIS is not entirely preventable, certain lifestyle modifications can help reduce the risk of progression:
- Maintaining a Healthy Weight: Obesity is associated with an increased risk of breast cancer.
- Regular Exercise: Physical activity can help reduce the risk of breast cancer.
- Limiting Alcohol Consumption: Excessive alcohol intake has been linked to an increased risk of breast cancer.
Research and Future Directions

The understanding of LCIS has significantly evolved, leading to a shift in focus from its initial classification as a benign condition to a more nuanced perspective recognizing its potential for progression to invasive breast cancer. Ongoing research is dedicated to unraveling the intricate molecular mechanisms underlying LCIS development and progression, paving the way for novel therapeutic interventions and improved patient management.
Molecular Mechanisms Underlying LCIS Progression
The molecular basis of LCIS progression remains a subject of active investigation. Recent research has shed light on key molecular alterations and pathways that contribute to the transition from non-invasive LCIS to invasive breast cancer. These findings provide valuable insights into the underlying biology of LCIS and hold promise for the development of targeted therapies.
- Genetic and Epigenetic Alterations: Researchers have identified specific genetic mutations and epigenetic modifications associated with LCIS progression. These include mutations in genes involved in cell growth and proliferation, such as TP53 and PTEN, as well as alterations in DNA methylation patterns. These findings suggest that genetic and epigenetic instability play a crucial role in the development and progression of LCIS.
- Microenvironment and Cell-Cell Interactions: The microenvironment surrounding LCIS cells has been implicated in disease progression. Studies have shown that interactions between LCIS cells and surrounding stromal cells, including fibroblasts and immune cells, can influence the growth and invasiveness of LCIS. This interplay involves the exchange of signaling molecules and the creation of a microenvironment conducive to tumor growth.
- Hormonal Influences: Estrogen and progesterone receptors are often expressed in LCIS cells, suggesting a role for hormonal influences in disease progression. Research is ongoing to understand how hormonal signaling pathways contribute to the development and progression of LCIS and to identify potential therapeutic targets for hormonal manipulation.
Novel Therapies and Targeted Interventions
The growing understanding of the molecular mechanisms underlying LCIS has paved the way for the development of novel therapies and targeted interventions. These approaches aim to prevent or delay the progression of LCIS to invasive breast cancer, offering personalized treatment options for patients at risk.
- Selective Estrogen Receptor Modulators (SERMs): SERMs, such as tamoxifen, have shown efficacy in reducing the risk of invasive breast cancer in women with LCIS. By blocking estrogen receptors, SERMs can inhibit the growth of estrogen-sensitive LCIS cells. However, SERMs are not without side effects, and their use should be carefully considered in consultation with a healthcare professional.
- Aromatase Inhibitors: Aromatase inhibitors, such as anastrozole and letrozole, are another class of drugs that target estrogen production. They can be effective in reducing estrogen levels and inhibiting the growth of estrogen-dependent LCIS cells. Aromatase inhibitors are often used in postmenopausal women with LCIS.
- Targeted Therapies: Advances in molecular biology have led to the development of targeted therapies that specifically target key molecular pathways involved in LCIS progression. For example, therapies targeting the PI3K/AKT/mTOR pathway, which is frequently dysregulated in LCIS, are under investigation. These therapies aim to block the signaling pathways that promote cell growth and survival in LCIS cells.
Challenges and Opportunities in LCIS Research, Does lobular carcinoma in situ invade stroma
While significant progress has been made in understanding LCIS, several challenges remain. Addressing these challenges will be crucial for advancing LCIS research and developing more effective treatments.
- Heterogeneity of LCIS: LCIS is a heterogeneous disease, with different subtypes exhibiting varying degrees of risk for progression to invasive cancer. This heterogeneity poses challenges for developing therapies that effectively target all subtypes of LCIS.
- Lack of Standardized Treatment Guidelines: Currently, there are no standardized treatment guidelines for LCIS, leading to variability in management strategies. This variability can hinder research efforts and make it difficult to compare treatment outcomes across different studies.
- Limited Clinical Trials: Clinical trials investigating the efficacy of different therapies for LCIS are often limited in size and scope. This makes it challenging to definitively evaluate the effectiveness of new treatments and to identify the best management strategies for different patient populations.
While LCIS doesn’t directly invade the stroma, its presence signals a heightened risk of developing invasive breast cancer. Early detection and careful monitoring are essential for managing LCIS. Ongoing research is focused on identifying the molecular mechanisms driving LCIS progression and developing targeted therapies to prevent or delay the development of invasive disease. Understanding the intricate relationship between LCIS and the surrounding stroma is crucial for improving breast cancer outcomes and providing effective patient care.
FAQ Resource: Does Lobular Carcinoma In Situ Invade Stroma
What are the symptoms of LCIS?
LCIS typically doesn’t cause any noticeable symptoms. It’s often detected during routine mammograms or biopsies performed for other reasons.
Is LCIS curable?
LCIS itself isn’t curable, but it can be managed effectively through surveillance and treatment options.
What are the treatment options for LCIS?
Treatment options for LCIS vary depending on individual risk factors and preferences. They may include close monitoring, medications, or surgery.






