What is benign endocervical glands and stroma – What are benign endocervical glands and stroma sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. The cervix, a vital part of the female reproductive system, plays a crucial role in protecting the uterus and facilitating childbirth. Within its intricate structure, we find the endocervical glands and stroma, tissues that are essential for the cervix’s normal functioning.
While these tissues typically remain healthy, they can sometimes undergo benign changes, which are non-cancerous alterations that can be observed under a microscope.
This exploration delves into the microscopic world of the cervix, examining the normal features of endocervical glands and stroma and exploring the various benign changes that can occur. We’ll uncover the nuances of simple and complex hyperplasia, the characteristics of endocervical polyps, and the microscopic appearances of fibromuscular hyperplasia and stromal fibrosis. Understanding these benign changes is crucial for accurate diagnosis and management, ensuring that any potential concerns are addressed promptly and effectively.
Introduction to Benign Endocervical Glands and Stroma
The cervix is the lower, narrow end of the uterus that connects to the vagina. It plays a crucial role in the reproductive system, acting as a barrier between the uterus and the external environment. The cervix is composed of two main types of tissue: the ectocervix and the endocervix. The ectocervix, the outer portion of the cervix, is lined by squamous epithelium, while the endocervix, the inner portion of the cervix, is lined by glandular epithelium.Endocervical glands are specialized glands that line the endocervical canal.
They are responsible for producing mucus, which plays a vital role in protecting the uterus from infection and aiding in sperm transport. The stroma, the supportive tissue surrounding the glands, provides structural support and contains blood vessels, nerves, and lymphatic channels.Benign changes in the endocervical glands and stroma are common and usually do not cause any symptoms. These changes can occur due to various factors, including hormonal fluctuations, inflammation, and infections.
Normal Structure and Function of Endocervical Glands and Stroma
The endocervical glands are tubular structures that extend into the stroma. They are lined by a single layer of columnar epithelial cells that secrete mucus. The mucus produced by the endocervical glands is thick and sticky, which helps to trap foreign particles and prevent them from entering the uterus. The mucus also changes in consistency throughout the menstrual cycle, becoming thinner and more watery during ovulation to facilitate sperm transport.The stroma surrounding the endocervical glands is composed of connective tissue, blood vessels, nerves, and lymphatic channels.
It provides structural support for the glands and helps to regulate their function.
Benign Changes in Endocervical Glands and Stroma
Benign changes in the endocervical glands and stroma are often asymptomatic and are usually discovered during routine pelvic examinations or Pap tests. These changes can include:
- Endocervical polyps: These are small, benign growths that protrude from the endocervical canal. They are often asymptomatic and can be easily removed during a routine examination.
- Nabothian cysts: These are small, fluid-filled cysts that form when the openings of endocervical glands become blocked. They are usually asymptomatic and do not require treatment.
- Cervical ectropion: This condition occurs when the glandular epithelium of the endocervix extends outward onto the ectocervix. It is usually asymptomatic but can cause abnormal bleeding or discharge.
- Cervical erosion: This refers to a superficial ulceration or breakdown of the cervical epithelium. It can be caused by inflammation, infection, or trauma.
- Cervical hyperplasia: This refers to an increase in the number of cells in the endocervical epithelium. It is usually benign but can sometimes be a precursor to cervical cancer.
These benign changes are generally not a cause for concern and are often monitored closely. However, it is important to note that some benign changes can be associated with an increased risk of cervical cancer. Therefore, regular Pap tests are essential for early detection and prevention.
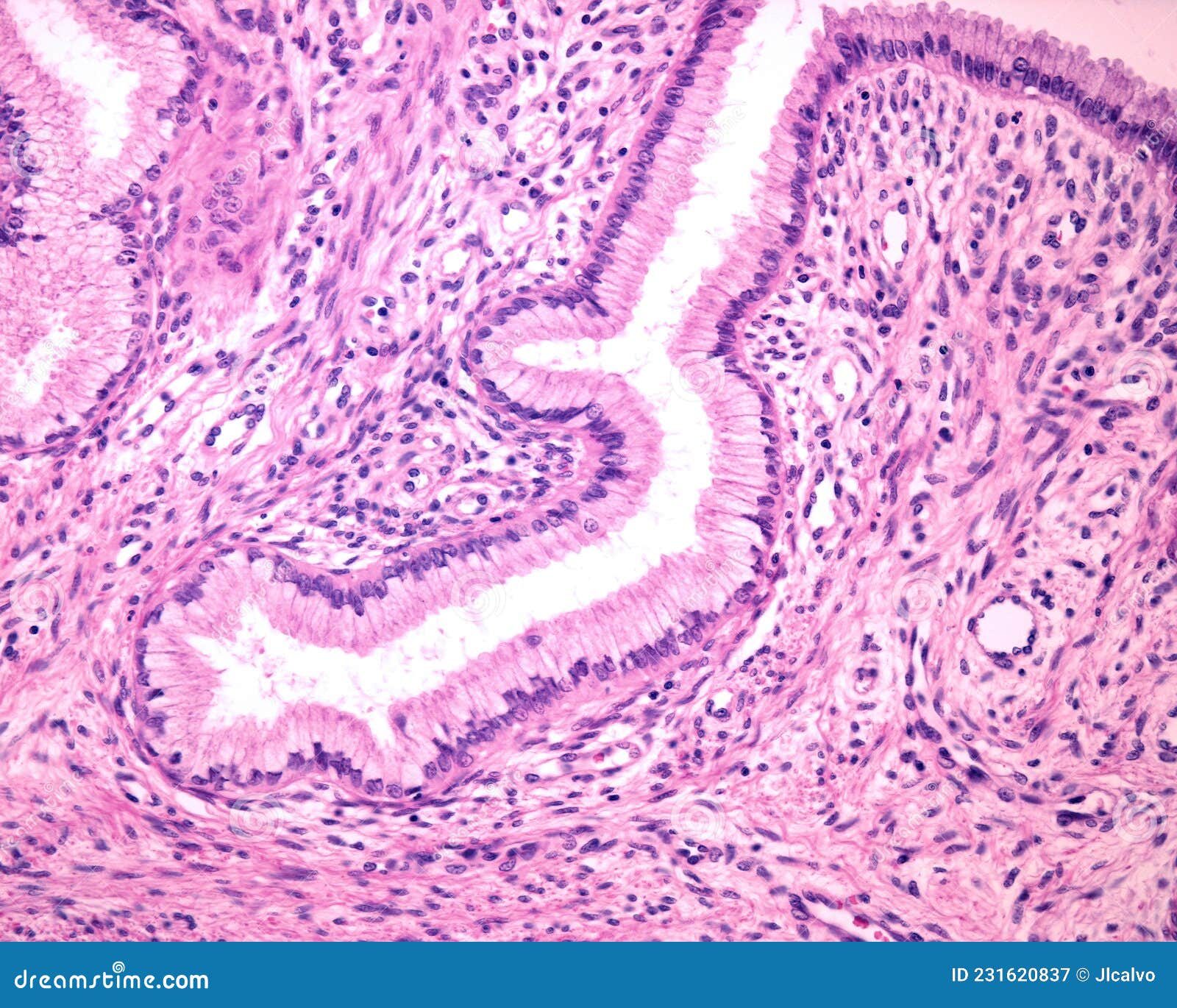
Microscopic Features of Benign Endocervical Glands
Microscopic examination of the cervix reveals the presence of endocervical glands, which are responsible for producing mucus. These glands are lined by a single layer of columnar epithelial cells, which are characterized by their tall, slender shape and basally located nuclei. The glands themselves are typically branched and have a characteristic appearance, with a central lumen surrounded by a layer of epithelial cells.The microscopic features of normal endocervical glands differ from those of atypical glands.
In normal glands, the epithelial cells are well-differentiated, with regular nuclei and a uniform appearance. The glands are also well-formed and organized, with a distinct lumen and a surrounding layer of epithelial cells. In contrast, atypical endocervical glands may show features such as:* Irregular gland shapes and sizes
- Disordered epithelial cell arrangement
- Nuclear atypia, including enlarged nuclei, hyperchromasia, and increased mitotic activity
Simple Hyperplasia, What is benign endocervical glands and stroma
Simple hyperplasia is a benign condition characterized by an increase in the number of endocervical glands. Microscopically, simple hyperplasia is characterized by an increase in the number of endocervical glands, but the glands themselves are typically well-formed and organized. The epithelial cells are usually well-differentiated, with regular nuclei and a uniform appearance. Simple hyperplasia is typically considered a low-grade lesion and is often associated with hormonal changes, such as those that occur during pregnancy or menopause.
Complex Hyperplasia
Complex hyperplasia is a more advanced form of hyperplasia, characterized by more significant changes in the endocervical glands. Microscopically, complex hyperplasia is characterized by an increase in the number of endocervical glands, as well as a more complex and irregular arrangement of the glands. The epithelial cells may show some degree of atypia, including enlarged nuclei and increased mitotic activity.
Complex hyperplasia is typically considered a higher-grade lesion than simple hyperplasia and is more likely to progress to cervical intraepithelial neoplasia (CIN).
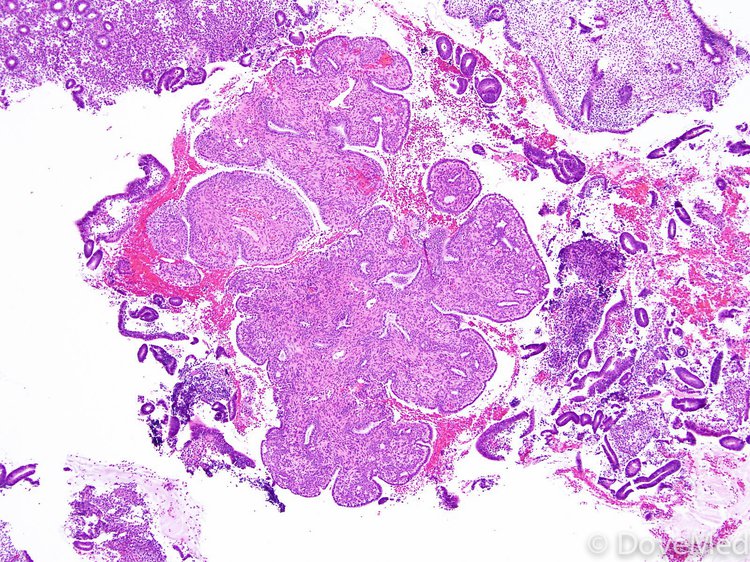
Endocervical Polyp
Endocervical polyps are benign growths that arise from the endocervical mucosa. Microscopically, endocervical polyps are characterized by a proliferation of endocervical glands and stroma. The glands are typically well-formed and organized, but they may be more numerous and crowded than in normal endocervical mucosa. The stroma is usually edematous and contains blood vessels and inflammatory cells. Endocervical polyps are typically asymptomatic and are often discovered during a routine pelvic examination.
Microscopic Features of Benign Endocervical Stroma
The endocervical stroma is the supportive connective tissue surrounding the endocervical glands. Its microscopic appearance is crucial for understanding the normal architecture of the cervix and recognizing any abnormalities.
Normal Endocervical Stroma
Under a microscope, normal endocervical stroma exhibits a loose, cellular appearance. It is composed primarily of fibroblasts, collagen fibers, and a network of blood vessels. The stroma is typically arranged in a delicate, interwoven pattern, with a moderate amount of ground substance. The cells within the stroma are typically small and spindle-shaped, with oval nuclei. The stroma is often described as having a “myxoid” appearance, meaning it has a slightly gelatinous or mucoid quality.
Differences Between Normal and Atypical Endocervical Stroma
Atypical endocervical stroma can be distinguished from normal stroma by several microscopic features. These include:
- Increased cellularity: Atypical stroma may show an increased number of cells, often with a more densely packed appearance.
- Nuclear atypia: The nuclei of cells in atypical stroma may be larger, more irregular in shape, or exhibit a more prominent nucleolus. This can be a sign of cellular proliferation or dysplasia.
- Increased fibrosis: Atypical stroma may show an increased amount of collagen fibers, giving it a more dense and fibrous appearance.
- Inflammation: Atypical stroma may show signs of inflammation, such as an increased number of inflammatory cells (e.g., lymphocytes, plasma cells, neutrophils).
Fibromuscular Hyperplasia
Fibromuscular hyperplasia is a benign condition characterized by an increase in the amount of smooth muscle and fibrous tissue in the endocervical stroma. This condition is often associated with hormonal changes, such as those that occur during pregnancy or menopause. Microscopically, fibromuscular hyperplasia is characterized by:
- Increased smooth muscle bundles: The stroma shows an increase in the number and size of smooth muscle bundles, which are often arranged in a whorled or concentric pattern.
- Increased collagen fibers: The stroma also shows an increase in the amount of collagen fibers, which may appear more dense and compact.
- Increased cellularity: There may be an increase in the number of fibroblasts and other stromal cells.
Stromal Fibrosis
Stromal fibrosis is a condition characterized by an excessive deposition of collagen fibers in the endocervical stroma. This can lead to a thickening and hardening of the stroma. Microscopically, stromal fibrosis is characterized by:
- Increased collagen fibers: The stroma shows a significant increase in the amount of collagen fibers, which may appear thick, dense, and hyalinized (glassy).
- Reduced cellularity: The stroma may show a decrease in the number of stromal cells.
- Narrowed gland lumens: The increased collagen fibers may compress and narrow the lumens of the endocervical glands.
Clinical Significance of Benign Endocervical Changes
Benign endocervical changes, while not inherently cancerous, can pose diagnostic challenges and require careful evaluation. Understanding their clinical significance is crucial for accurate diagnosis and appropriate management.
Potential for Misdiagnosis
Benign endocervical changes can sometimes mimic the appearance of precancerous or cancerous lesions under the microscope. This can lead to unnecessary anxiety and potentially aggressive treatment. The resemblance can arise from various factors, including:
- Increased cellular activity: Benign endocervical glands can exhibit increased cellular proliferation, mimicking the appearance of precancerous lesions.
- Inflammation: Chronic inflammation can cause changes in the endocervical epithelium, making it difficult to distinguish from dysplasia or cancer.
- Hormonal influences: Hormonal fluctuations can affect the appearance of the endocervical glands, leading to atypical features.
Importance of Accurate Diagnosis and Management
Accurate diagnosis of benign endocervical changes is essential to avoid unnecessary treatment and ensure proper patient care.
- Avoidance of overtreatment: Misdiagnosis can lead to unnecessary biopsies, colposcopies, or even surgical interventions, which can have associated risks and costs.
- Monitoring and follow-up: Correctly identifying benign changes allows for appropriate monitoring and follow-up, ensuring early detection of any potential progression.
- Patient reassurance: Accurate diagnosis provides reassurance to patients, reducing anxiety and unnecessary stress.
Differential Diagnosis of Benign Endocervical Changes
Accurate diagnosis of cervical lesions is crucial for appropriate management and to prevent the progression of precancerous changes to invasive cancer. Distinguishing benign endocervical changes from precancerous and cancerous lesions is essential.
Microscopic Features for Differentiation
The microscopic features of benign endocervical changes differ significantly from those of precancerous and cancerous lesions. Here’s a comparison:
Benign Endocervical Changes
- Regular, well-defined glands with a single layer of columnar epithelial cells.
- Glands are evenly distributed and exhibit a normal, non-proliferative pattern.
- Stroma is loose and cellular, with a normal vascular pattern.
- Absence of atypical cells or nuclear abnormalities.
Precancerous Lesions (Cervical Intraepithelial Neoplasia – CIN)
- Disordered epithelial architecture with abnormal cell growth and maturation.
- Increased nuclear size and hyperchromasia (increased nuclear staining).
- Loss of normal cell polarity and stratification.
- Presence of atypical cells with mitotic figures (cell division) in abnormal locations.
Cancerous Lesions (Cervical Cancer)
- Invasive growth of malignant cells beyond the basement membrane.
- Markedly abnormal cellular morphology with increased nuclear atypia and mitotic figures.
- Disruption of normal tissue architecture and invasion into surrounding tissues.
- Possible presence of necrosis (cell death) and inflammatory cells.
Key Features for Differentiation
- Regularity of Glandular Architecture: Benign changes exhibit well-defined, regular glands, while precancerous and cancerous lesions show disordered architecture.
- Nuclear Morphology: Benign cells have normal nuclei, while precancerous and cancerous cells exhibit increased nuclear size, hyperchromasia, and atypical features.
- Cell Proliferation: Benign changes show a normal, non-proliferative pattern, while precancerous and cancerous lesions exhibit abnormal cell growth and proliferation.
- Invasion: Benign changes remain confined to the epithelium, while cancerous lesions invade surrounding tissues.
Table Summarizing Key Differences
| Feature | Benign | Precancerous (CIN) | Cancerous (Cervical Cancer) |
|---|---|---|---|
| Glandular Architecture | Regular, well-defined | Disordered, abnormal | Disrupted, invasive |
| Nuclear Morphology | Normal | Atypical, hyperchromatic | Markedly atypical |
| Cell Proliferation | Normal, non-proliferative | Increased, abnormal | Rapid, invasive |
| Invasion | None | None | Present |
Management of Benign Endocervical Changes: What Is Benign Endocervical Glands And Stroma
Benign endocervical changes, while generally not concerning, may require management depending on their severity and the patient’s individual circumstances. The primary goal is to monitor for any potential progression to precancerous or cancerous lesions.
Management Options for Benign Endocervical Changes
The management of benign endocervical changes typically involves a combination of observation, follow-up, and, in some cases, treatment. The specific approach will depend on the type of change, its severity, and the patient’s overall health and risk factors.
Observation and Follow-Up
Observation and follow-up are often the initial steps in managing benign endocervical changes. This involves regular cervical cancer screenings, such as Pap smears, to monitor for any changes over time. The frequency of follow-up visits will depend on the specific type of change and the patient’s individual risk factors. For example, women with a history of abnormal Pap smears or HPV infection may require more frequent follow-up.
Treatment
Treatment for benign endocervical changes is usually reserved for cases that are persistent, severe, or associated with symptoms. Treatment options may include:
- Cryotherapy: This involves freezing the affected tissue with liquid nitrogen, destroying abnormal cells. Cryotherapy is often used for mild to moderate changes and is generally well-tolerated.
- LEEP (Loop Electrosurgical Excision Procedure): This is a minimally invasive procedure that uses a heated wire loop to remove abnormal tissue. LEEP is typically used for more severe changes or when there is a concern about precancerous lesions.
- Conization: This procedure involves removing a cone-shaped piece of tissue from the cervix. Conization is usually reserved for larger or more complex lesions. It may be performed as a diagnostic or therapeutic procedure.
Table of Management Options
| Type of Change | Recommended Approach | Potential Risks and Benefits |
|---|---|---|
| Mild, isolated changes | Observation and follow-up with Pap smears | Benefits: Minimal risk, allows for monitoring of changes. Risks: Potential progression to more severe changes if not closely monitored. |
| Moderate to severe changes, persistent changes, or changes with symptoms | Treatment with cryotherapy, LEEP, or conization | Benefits: Removal of abnormal tissue, reduced risk of progression to cancer. Risks: Complications such as bleeding, infection, or cervical stenosis. |
Illustrative Cases
Illustrative cases provide a practical understanding of benign endocervical changes and how they are diagnosed and managed in clinical settings.
Case Scenario
A 35-year-old woman presents to her gynecologist for a routine Pap smear. The Pap smear results show atypical squamous cells of undetermined significance (ASC-US). The patient has no significant medical history and reports no abnormal vaginal bleeding or discharge.
Diagnostic Process
Following the ASC-US Pap smear result, the gynecologist recommends a colposcopy to further evaluate the cervical cells. Colposcopy involves using a magnifying device to visualize the cervix and allows for the identification of any abnormal areas. During the colposcopy, a small biopsy is taken from the suspicious area for microscopic examination.
Microscopic Features
The biopsy reveals the presence of endocervical glands and stroma. The glands are lined by a single layer of columnar epithelial cells with a basally located nucleus and abundant cytoplasm. The stroma surrounding the glands is composed of loose connective tissue with a rich vascular network. The cells in the stroma are spindle-shaped and arranged in a haphazard fashion.
Management
Based on the microscopic findings, the patient is diagnosed with benign endocervical changes. The management of this condition is typically conservative and involves close monitoring. The patient will be advised to undergo regular Pap smears every 6-12 months to monitor for any changes in the cervical cells.
The journey through the microscopic world of the cervix reveals the intricate interplay of normal and benign changes in endocervical glands and stroma. While these alterations are generally non-cancerous, it’s essential to recognize their potential for mimicking precancerous or cancerous lesions. This emphasizes the importance of accurate diagnosis, which can guide appropriate management strategies, ensuring the well-being of patients. By unraveling the mysteries of benign endocervical changes, we gain a deeper appreciation for the complexities of the cervix and its vital role in female health.
Expert Answers
What is the most common type of benign endocervical change?
Simple hyperplasia is the most commonly observed benign change in endocervical glands.
Are benign endocervical changes always visible on a Pap smear?
Not necessarily. Some benign changes might not be apparent on a Pap smear, while others may show up as atypical glandular cells. Further investigation with a colposcopy and biopsy is often needed for a definitive diagnosis.
What are the long-term implications of benign endocervical changes?
Most benign endocervical changes are harmless and don’t pose any long-term health risks. However, some changes, like complex hyperplasia, may have a slightly increased risk of developing cervical cancer in the future, making regular follow-up appointments crucial.
Is treatment always necessary for benign endocervical changes?
Treatment is not always required for benign endocervical changes. In many cases, close observation and follow-up are sufficient. However, if the changes are concerning or cause symptoms, treatment options like excision or ablation may be considered.






